Teeth diseases and treatment
This comprehensive review aims to provide an in-depth understanding of the anatomy of teeth, the various dental diseases that can affect them, and the available treatments to manage these conditions. The information provided will serve as a valuable resource for dental professionals and those interested in understanding more about dental health.

I. Introduction
A. Importance of Dental Health
Dental health is an essential aspect of overall health and well-being. Good oral hygiene practices and regular dental check-ups can help prevent the development of dental diseases, which can lead to pain, tooth loss, and even systemic health issues if left untreated. Maintaining proper dental health is crucial for several reasons:
a. Chewing and Digestion: Healthy teeth are necessary for efficient chewing, which is the first step in the digestion process. Chewing breaks down food into smaller particles, allowing for better nutrient absorption in the gastrointestinal tract.
b. Speech: Teeth play a critical role in speech production, particularly in the pronunciation of certain sounds. Dental problems, such as tooth loss or misalignment, can affect speech clarity and lead to communication difficulties.
c. Aesthetics and Self-esteem: A healthy and attractive smile is often seen as a sign of good health, enhancing one’s self-confidence and social interactions. Dental issues like discolored or missing teeth can negatively impact a person’s self-esteem.
d. Systemic Health: Poor dental health has been linked to various systemic health issues, including heart disease, diabetes, respiratory infections, and even pregnancy complications. Oral bacteria can enter the bloodstream, causing inflammation and affecting other organs in the body.

B. Overview of Tooth Anatomy and Dental Diseases
Understanding the basic anatomy of teeth is crucial for recognizing dental diseases and knowing how to address them effectively. This article will cover the structure and function of teeth, the different types of teeth, and their development and eruption. Additionally, we will delve into various dental diseases, their causes, symptoms, and prevention strategies, and explore the treatments available for managing these conditions.
II. Tooth Anatomy
A. Basic Structure of Teeth
Teeth are complex structures designed to perform various functions, such as biting, tearing, and grinding food. The primary components of a tooth are enamel, dentin, pulp, and cementum.
-
Enamel: Enamel is the outermost layer of the tooth, composed of highly mineralized tissue. It is the hardest substance in the human body, even harder than bone. The primary function of enamel is to protect the tooth from wear and tear during chewing and to provide a barrier against temperature fluctuations and chemicals.
-
Dentin: Dentin is the layer beneath the enamel, forming the bulk of the tooth structure. It is a porous, calcified tissue that is softer than enamel but harder than bone. Dentin provides support to the enamel and acts as a protective layer for the tooth’s inner pulp.
-
Pulp: Pulp is the innermost part of the tooth, consisting of blood vessels, nerves, and connective tissue. It is responsible for nourishing the tooth and providing sensory perception, such as detecting temperature changes and pain. The pulp extends from the crown of the tooth to the root, through a narrow channel called the root canal.
-
Cementum: Cementum is a thin layer of calcified tissue covering the tooth’s root. It connects the tooth to the periodontal ligament, which anchors the tooth to the alveolar bone in the jaw. Cementum plays a crucial role in maintaining the stability and position of the tooth within the jawbone.
B. Types of Teeth
There are four types of teeth in the human dentition, each with a specific function:
-
Incisors: Incisors are the front teeth, located in the central part of the upper and lower jaws. They have a flat, chisel-like edge and are designed for biting and cutting food into smaller pieces. There are eight incisors in total, with four in the upper jaw and four in the lower jaw.
-
Canines: Canines, also known as cuspids, are located next to the incisors. They have a sharp, pointed edge and are used for tearing and ripping food. There are four canines, with two in the upper jaw and two in the lower jaw.
-
Premolars: Premolars, or bicuspids, are located between the canines and molars. They have two cusps on their chewing surface and are used for crushing and grinding food. There are eight premolars in total, with four in the upper jaw and four in the lower jaw.
-
Molars: Molars are the largest teeth, located at the back of the mouth. They have a broad, flat chewing surface with multiple cusps, allowing them to grind food into a fine consistency. There are twelve molars in total, with six in the upper jaw and six in the lower jaw. The third molars, also known as wisdom teeth, are the last to erupt and often cause problems due to insufficient space in the jaw.
C. Tooth Development and Eruption
Tooth development begins in the embryonic stage, with the formation of tooth buds that eventually give rise to the various tooth components. The process of tooth eruption, or the emergence of teeth through the gums, occurs in stages throughout childhood and adolescence.
-
Primary Teeth: Primary teeth, also known as baby teeth or deciduous teeth, begin to develop in the womb and start to erupt around six months of age. There are 20 primary teeth in total, and they play a crucial role in guiding the permanent teeth into their correct positions.

III. Dental Diseases
A. Dental Caries
-
Causes: Dental caries, commonly known as tooth decay or cavities, are caused by the demineralization of tooth enamel and dentin by acids produced by bacteria in the mouth. The primary culprit is Streptococcus mutans, which thrives on sugars and carbohydrates in the diet. As these bacteria metabolize the sugars, they produce acids that break down the tooth’s mineral content, eventually leading to the formation of a cavity.
-
Symptoms: Early stages of dental caries may not exhibit any noticeable symptoms. However, as the decay progresses, the following symptoms may appear:
- White or brown spots on the tooth surface
- Tooth sensitivity to hot, cold, or sweet foods and beverages
- Toothache or spontaneous pain in the tooth
- Pain when biting or chewing
- Visible holes or pits in the tooth
-
Prevention: Preventing dental caries involves maintaining good oral hygiene practices and making dietary modifications. Some prevention strategies include:
- Brushing teeth at least twice a day with fluoride toothpaste
- Flossing daily to remove plaque and food particles between teeth
- Regular dental check-ups and cleanings
- Consuming a balanced diet and limiting sugary foods and beverages
- Drinking fluoridated water or using fluoride mouth rinses
- Applying dental sealants to protect the chewing surfaces of molars
B. Periodontal Diseases
-
Gingivitis: Gingivitis is a mild form of periodontal disease characterized by inflammation of the gums (gingiva) due to plaque buildup. Symptoms of gingivitis include red, swollen gums that bleed easily during brushing or flossing. Gingivitis can be reversed with proper oral hygiene practices and professional dental cleanings.
-
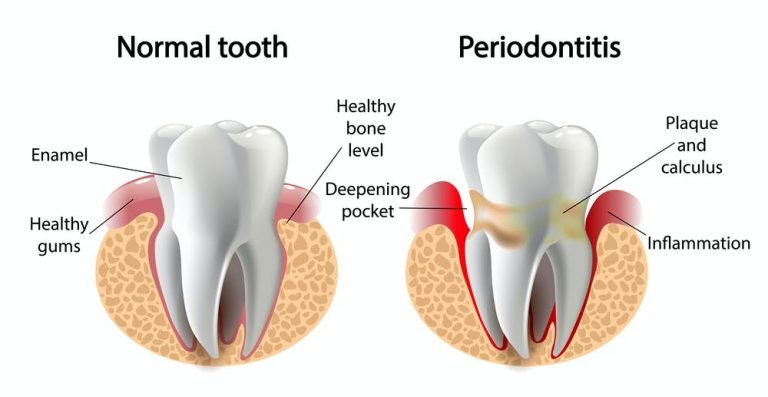
Periodontitis: If left untreated, gingivitis can progress to periodontitis, a more severe form of periodontal disease that affects the supporting structures of the teeth, including the periodontal ligament and alveolar bone. Periodontitis can lead to tooth mobility, gum recession, and eventual tooth loss. Symptoms of periodontitis include:
- Persistent bad breath
- Gums that bleed easily
- Red, swollen, or tender gums
- Receding gums or teeth that appear longer
- Pus between the teeth and gums
- Loose or shifting teeth
-
Risk Factors and Prevention: Several factors can increase the risk of developing periodontal diseases, such as poor oral hygiene, tobacco use, genetics, diabetes, hormonal changes, and certain medications. Prevention strategies for periodontal diseases include:
- Brushing and flossing daily to remove plaque and bacteria
- Regular dental check-ups and professional cleanings
- Eating a balanced diet rich in vitamins and minerals
- Quitting tobacco use
- Managing underlying health conditions, such as diabetes
C. Oral Cancer
-
Risk Factors: Oral cancer can affect any part of the oral cavity, including the lips, tongue, cheeks, gums, floor of the mouth, and palate. Factors that increase the risk of oral cancer include tobacco use, excessive alcohol consumption, human papillomavirus (HPV) infection, exposure to ultraviolet (UV) light, and a diet low in fruits and vegetables.
-
Symptoms: Symptoms of oral cancer can vary depending on the location and stage of the disease. Some common signs and symptoms include:
- A persistent sore or ulcer in the mouth that does not heal
- A lump or thickening in the cheek or gums
- White or red patches in the mouth
IV. Dental Treatments
A. Diagnosis and Prevention
-
Regular Dental Check-ups: Regular dental visits are essential for maintaining optimal oral health. Dentists can detect early signs of dental diseases and provide appropriate treatments to prevent further complications. It is recommended to visit the dentist every six months for check-ups and professional cleanings.
-
Dental Radiography: Dental X-rays are an essential diagnostic tool that allows dentists to detect dental diseases and abnormalities that may not be visible during a clinical examination. X-rays can reveal issues such as tooth decay, bone loss, impacted teeth, and dental infections.
-
Oral Hygiene Education: Dentists and dental hygienists play a crucial role in educating patients about proper oral hygiene practices, including correct brushing and flossing techniques, dietary modifications, and the importance of regular dental visits.
B. Restorative Treatments
-
Dental Fillings: Dental fillings are a common treatment for cavities caused by tooth decay. The decayed tooth material is removed, and the cavity is filled with a dental material such as composite resin, amalgam, gold, or porcelain to restore the tooth’s structure and function.
-
Dental Crowns: Dental crowns, also known as caps, are used to restore teeth that are severely damaged, decayed, or discolored. A crown is a custom-made restoration that covers the entire visible portion of the tooth, providing strength and improving its appearance.
-
Dental Bridges: Dental bridges are used to replace one or more missing teeth. A bridge consists of artificial teeth (pontics) supported by dental crowns placed on the adjacent natural teeth or dental implants. Bridges help restore function and aesthetics in areas with missing teeth.
-
Root Canal Treatment: Root canal treatment, also known as endodontic therapy, is a procedure used to save a severely damaged or infected tooth. The infected pulp tissue is removed, the root canal system is cleaned and disinfected, and the tooth is sealed with a filling material. A dental crown is often placed to protect and strengthen the tooth after the procedure.
C. Periodontal Treatments
-
Scaling and Root Planing: Scaling and root planing, also known as deep cleaning, is a non-surgical periodontal treatment used to remove plaque and calculus (tartar) from the tooth’s surface and below the gumline. This procedure helps to reduce inflammation and promote the healing of the gum tissue.
-
Periodontal Surgery: In cases of advanced periodontitis or when non-surgical treatments are not sufficient, periodontal surgery may be necessary to restore the health of the gums and supporting structures of the teeth. Some common periodontal surgeries include flap surgery (pocket reduction), bone grafting, and guided tissue regeneration.
-
Dental Implants: Dental implants are an effective solution for replacing missing teeth. A dental implant consists of a titanium post that is surgically placed into the jawbone, acting as an artificial tooth root. Once the implant has integrated with the bone, a dental crown, bridge, or denture can be attached to the implant, providing a stable and natural-looking tooth replacement.
D. Oral and Maxillofacial Surgery
-
Tooth Extractions: Tooth extractions may be necessary for various reasons, such as severe tooth decay, gum disease, impacted wisdom teeth, or orthodontic treatment. Extractions can be either simple (performed with dental forceps) or surgical (requiring an incision in the gum tissue and bone removal).
-
Treatment of Oral Cancer: Oral and maxillofacial surgeons play a crucial role in the diagnosis and treatment of oral cancer. Treatment options for oral cancer include surgery to remove the tumor, radiation therapy, chemotherapy, and targeted drug therapy.

V. Orthodontics and Dentofacial Orthopedics
A. Malocclusion and Its Effects
-
Definition: Malocclusion refers to the misalignment of teeth or an improper bite. This condition can lead to several issues, such as difficulty in chewing, speech problems, increased risk of tooth decay and gum disease, temporomandibular joint (TMJ) disorders, and aesthetic concerns.
-
Causes: Malocclusion can be caused by various factors, including genetics, childhood habits (e.g., thumb sucking, prolonged use of a pacifier), dental trauma, or premature loss of primary teeth.
B. Orthodontic Treatments
-
Braces: Braces are the most common orthodontic treatment used to correct malocclusion. They consist of brackets bonded to the tooth surface, archwires connecting the brackets, and elastic bands to apply pressure. Braces gradually move the teeth into their desired positions by exerting continuous force on them.
-
Clear Aligners: Clear aligners, such as Invisalign, are an alternative to traditional braces for treating mild to moderate orthodontic issues. They are custom-made, removable plastic trays that apply gentle pressure to reposition the teeth. Aligners are virtually invisible and can be removed for eating, brushing, and flossing.
-
Orthodontic Appliances: Various orthodontic appliances may be used alongside braces or clear aligners to correct specific problems, such as palate expanders to widen the upper jaw, headgear to control the growth of the upper and lower jaws, or retainers to maintain the teeth in their new positions after treatment.
C. Dentofacial Orthopedics
-
Definition: Dentofacial orthopedics is a specialized field within orthodontics that focuses on the growth and development of the facial bones and the alignment of the jaws. Dentofacial orthopedic treatments aim to correct jaw imbalances and promote harmonious facial growth.
-
Treatments: Dentofacial orthopedic treatments may involve the use of functional appliances, such as activators, twin blocks, or Herbst appliances, to modify the growth of the jaws and correct skeletal discrepancies. In some cases, orthognathic surgery may be necessary to reposition the jaws and achieve optimal facial balance and function.
D. Importance of Early Intervention
-
Early Orthodontic Evaluation: The American Association of Orthodontists recommends that children have their first orthodontic evaluation by the age of seven. Early detection and intervention of orthodontic issues can prevent more severe problems from developing and may reduce the need for extensive treatments later in life.
-
Interceptive Orthodontics: Interceptive orthodontics, also known as Phase I treatment, is performed during the mixed dentition stage (when both primary and permanent teeth are present). This approach may involve the use of orthodontic appliances or early extractions to address issues such as crossbites, crowding, or excessive overbites, and to guide the growth of the jaws and the eruption of the permanent teeth.