myths and facts about depression and anxiety
What is depression? Everything about depression, symptoms and treatments : A large portion of the population is affected by depression. We must be aware of this condition.
History of depression:
Humans have struggled with depression throughout history. Throughout history, depression has been recognized as a health problem by therapists, philosophers, and writers. In addition, they describe people’s persistent and intelligent efforts to find solutions to this problem.
Depression was originally called melancholia. Ancient Mesopotamian texts first mention melancholy in the second millennium BC. At this time, people believed all mental illnesses resulted from being possessed by demons. Priests treated these illnesses. Separate groups of physicians treated physical injuries, but not conditions such as depression.
Ancient Greeks and Romans saw melancholy in different ways. Literature of the time suggested that mental illness was caused by ghosts or demons. Greek historian Herodotus wrote about a king who had gone mad because of evil spirits about 400 BC.
Babylonian, Chinese, and Egyptian civilizations also considered mental illness to be a form of demon possession. Sex techniques such as beatings, restraints, and starvation were used. The purpose of these treatments was to drive the demons from the body of the infected person. In contrast, ancient Roman and Greek physicians considered depression to be a biological and mental illness. To treat depressive symptoms, gymnastics, massage, special diets, music, baths, and poppy extract and donkey milk were used.
Hippocrates, the Greek physician, believed that personality traits and mental illnesses are related to fluid imbalance. There were four types of fluids: yellow bile, black bile, phlegm, and blood. Hippocrates classified mental illnesses such as mania, melancholy, and Bersama. Melancholia was believed to be caused by too much black bile in the spleen. To treat the disease, he used cupping, bathing, exercise, and diet.
The famous Roman philosopher and politician Cicero argued that melancholy was caused by intense grief, fear, or anger, as opposed to Hippocrates’ views. It was a psychological explanation for depression instead of a physical one. Hippocrates’ influence diminished in the last years before Christ. In the view of educated Romans, demons and the gods’ wrath caused mental illnesses such as depression. Aulus Cornelius Celsus, for example, suggested starvation and confinement to treat the disease.
In contrast, the Baghdad hospital’s chief physician, Iranian Zakaria Razi, saw the brain as a place of mental illness and melancholy. Her mental illness treatments often included hydrotherapy (baths) and behavioral therapy (positive rewards for appropriate behavior).
After the fall of the Roman Empire, scientific thinking about mental illness and depression began to return. Throughout Europe, religious beliefs, especially Christianity, dominated other explanations for mental illness during the Middle Ages. Mentally ill people were thought to be possessed by demons, evil spirits, or witches.
Some physicians still believed that mental illness is caused by an imbalance of body fluids, a poor diet, and sadness. Psychiatric hospitals treated people with depression. In the 14th century, the Renaissance spread throughout Europe. During this period, thinking about mental illness was both progressive and regressive. In Europe, witch hunts and the execution of the mentally ill were quite common. Meanwhile, some physicians returned to Hippocrates’ view which held that mental illnesses were caused by natural causes and that those who were stigmatized and persecuted as witches needed compassionate medical treatment.
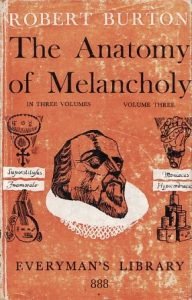
Robert Burton described the psychological and social causes of depression in 1621 in his book The Anatomy of Melancholy. Among these causes were poverty, fear, and social isolation. According to him, diet, exercise, distraction, detoxification, cupping, herbal remedies, marriage, and even music therapy are effective treatments for depression.
Depression was believed to be an inherited mood disorder at the beginning of the Enlightenment. The result was the exclusion of these patients from society and their homelessness and poverty. Physicians theorized that aggression was at the root of the problem at the end of the Enlightenment. Exercise, diet, music, and medication were prescribed, and doctors suggested the patient talk to a friend or physician about their problems. Doctors sometimes refer to depression as a conflict between “what you want” and “what you know is right.” Others continue to seek to identify the physical causes.
There were several Enlightenment treatments for depression, including water immersion (people were kept underwater as much as possible without drowning) and standing on a rotating platform to believe that the movement would “place” the brain’s contents. During this period, Benjamin Franklin also developed an early form of electroconvulsive therapy. Horseback riding, diet, cleansing, and vomiting were also recommended treatments.
In 1895, the German psychiatrist Emile Kriplin became the first to distinguish mania depression (what we now know as bipolar disorder) from premature insanity (a term used at the time for schizophrenia). The theory of psychoanalysis and psychoanalysis were developed during this period.
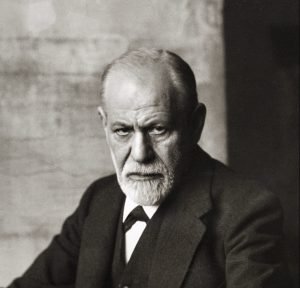
As early as 1917, Sigmund Freud wrote about mourning and melancholy, describing melancholy as a reaction to loss (such as a death) . Additionally, Freud believed that one’s subconscious anger about this loss leads to hateful and hurtful behavior toward oneself. In his opinion, psychoanalysis could resolve these unconscious conflicts and reduce self-harming thoughts and behaviors. During this time, however, physicians regarded depression as a brain disorder.

Generalized treatments for major depression were not designed to help patients in the late 19th and early 20th centuries, leading many patients who became frustrated with these treatments to undergo a lobotomy. The frontal part of their brain was destroyed during this surgery. The surgery was thought to relieve their symptoms. It is unfortunate that lobotomies often result in personality changes, loss of decision-making power, impaired judgment, and even death.

Patients with depression were sometimes treated with electroconvulsive therapy, an electric shock applied to the scalp to cause seizures.
Physicians classified depression into two subtypes in the 1950s and 1960s: endogenous (of physical origin) and neurological (environmental). Genetics or some other physical defect seemed to be the cause of endogenous depression. Conversely, the neurological or reactive type was thought to be caused by an external problem such as death or job loss.
The 1950s were a critical decade for the treatment of depression. It was at this time that doctors discovered a tuberculosis drug called isoniazid effectively treated depression in some people. Since then, drug therapies have been considered. As well, new schools of thought have emerged, such as the theory of family systems and cognitive-behavioral systems.
Presently, depression is believed to be caused by a variety of factors, including biological, psychological, and social factors. Psychotherapy and drugs that target neurotransmitters are generally preferred treatments. Electroconvulsive therapy is also used in certain conditions, such as refractory depression and severe cases that require immediate relief. The brain’s magnetic stimulation through the skull and vagus nerve stimulation, developed in recent years to help people who do not respond to medication or treatment, are newer therapies as well. There is no single treatment that works for everyone because the causes of depression are more complex than we realize.
Below is a brief overview of major depressive disorder:
Major depressive disorder (MDD), also known as depression, is characterized by a persistent low mood for at least two weeks in most cases. This condition is often characterized by low self-esteem, decreased interest in normally enjoyable activities, low energy, and pain without apparent cause. People who are affected by mental illness may sometimes see or hear things that do not exist externally. Between periods of depression, a few years are normal, while others experience these symptoms almost constantly.
Major depressive disorder can adversely affect a person’s personal, professional, academic, sleeping, and eating habits, as well as their general health. About 50% of people who die by suicide suffer from depression or another mood disorder, and between 2% and 8% of adults with depression commit suicide.
This disease is likely caused by a combination of genetic, environmental, and psychological factors. A family history of the disease, significant life changes, certain medications, chronic health problems, and substance abuse are risk factors. Self-reported experiences and a mental health test are used to diagnose depression. Major depression cannot be diagnosed by laboratory tests. Tests may be performed to rule out physical illnesses that cause similar symptoms. In contrast to feeling sad, which is a natural emotion, major depression is more severe and lasts longer.
It is usually treated with counseling and antidepressants. Cognitive behavioral therapy and interpersonal psychotherapy are two types of therapy. Electroconvulsive therapy may be used if other measures are unsuccessful. There may be a need for hospitalization where there is a risk of self-harm, which is sometimes done against the person’s wishes.
About 216 million people suffered from major depression in 2015. In France, 21% of people are affected, while in Japan, 7% are. Women get approximately twice as much as men.
In 1980, the American Psychiatric Association included Major Depressive Disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM). Major depression was included in the DSM-II version as a subtype of psychotic depression, which also included conditions now recognized as mood disorders (depressive disorder and mood disorder).
Symptoms of depression include :
Major depression has an impact on family and personal relationships, work or study life, sleep and eating behaviors, and general health. In people with depression, they usually experience a low mood that permeates all aspects of their lives and the inability to enjoy previously enjoyable activities.
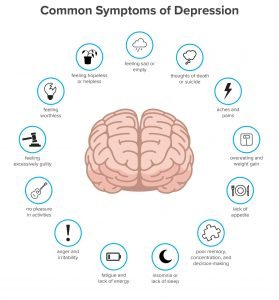
People who are depressed may feel worthless, remorseful, guilty, frustrated, and disgusted. They may also develop psychotic symptoms. These symptoms may include hallucinations and delusions. Low concentration and memory are other signs of depression, as are withdrawal from social activities and situations, decreased sexual desire, irritability, and thoughts of death or suicide.
Depression is also associated with insomnia. The person wakes up too early and cannot sleep again. Depression may also be accompanied by physical symptoms such as fatigue, headaches, and digestive problems. It is common for appetite to be reduced, which leads to weight loss, although there may also be an increase in appetite and weight gain.
As a result of depression, older adults may experience cognitive symptoms such as forgetfulness and noticeable slowness of movement. Physical disorders such as stroke, heart disease, Parkinson’s disease, and chronic obstructive pulmonary disease are often associated with depression in the elderly.
The symptoms of depressed children may vary depending on their age and circumstances, such as irritability instead of depressed behavior. Many of them lose interest in school and suffer from academic failure. They may be characterized as dependent and insecure. When these symptoms are mistaken for mood swings, the diagnosis of depression will be delayed, or the child may not even be diagnosed with depression.
Depressive disorders include:
Depression is often accompanied by other psychiatric disorders. In the US National Combination Survey, half of people with depression suffer from anxiety and related disorders, such as generalized anxiety disorder. Symptoms of anxiety can have a significant impact on depression and result in a delayed recovery, increased risk of recurrence, increased disability, and increased suicide risk.
About one-third of people diagnosed with Attention Deficit Hyperactivity Disorder also suffer from depression. These people are more likely to abuse substances, to become addicted to alcohol, and to develop other addictions.
They are also more likely to suffer from depression and pain. Approximately 65% of depressed people have one or more pain symptoms, and around 5 to 85% of people with pain also suffer from depression, depending on their condition. Depression is also linked to an increased risk of cardiovascular disease and to factors such as smoking and obesity. Depression increases a person’s risk of other medical problems because depressed people are less likely to follow medical guidelines for treating and preventing cardiovascular disease. In addition, a cardiologist may not notice that the patient is depressed behind the scenes of their cardiovascular problem.
Causes of depression :
Significant depression remains an enigma. Models of biopsychology suggest that biological, psychological, and social factors all contribute to depression.
Hereditary stress vulnerability theory says depression occurs when stressful life events trigger a pre-existing vulnerability. A history of vulnerabilities may be genetic, reflecting the interaction between heredity and environment, or it may be patterned and the result of worldviews acquired in childhood. Abuse, whether physical, sexual, or psychological, is a risk factor for this disease. The severity of depression, failure to respond to treatment, and illness duration are also associated with childhood trauma. However, some people are more prone to mental health problems, such as post-traumatic stress disorder, and several genes have been implicated in controlling this sensitivity.
The role of genetic factors in the incidence of depression:
Numerous genetic factors contribute to major depressive disorder, as with many other psychiatric disorders. A genome-level correlation study identified 44 genomic variants associated with depression risk. This study was followed in 2019 by another that identified 102 gene variants associated with depression. Based on this information, scientists calculate an individual score to assess a person’s genetic predisposition to this illness. This score explains only a small part of individual differences in depression risk.
Relationship between health problems and depression:

Secondary depression is caused by chronic or incurable diseases such as HIV, AIDS, or asthma. There is no certain way to determine whether behind-the-scenes disease causes depression through effects on quality of life or through common causes .
Some medications can also cause depression, such as this illness caused by certain medications. This illness may be caused by interferons, beta-blockers, isotretinoin, contraceptives, heart disease medications, anticonvulsants, anti-migraine medications, antipsychotic medications, and hormonal agents such as the releasing hormone gonadotropin agonist.
During pregnancy, depression is called postpartum illness and is thought to be caused by hormonal changes. An illness called Seasonal Affective Disorder is associated with seasonal changes in sunlight and appears to be a consequence of reduced sunlight.
Pathophysiology of depression :
The pathophysiology of this illness is not fully understood. The current theories revolve around monoaminergic systems, circadian rhythms, immunological disorders, hypothalamic-pituitary-adrenal axis disorders, and structural and functional abnormalities of emotional circuits.
The monoamine theory, which arose from monoaminergic drugs used to treat this illness, was the dominant theory until recently.
Monoamine neurotransmitters are believed to be the leading cause of this illness. Various studies support this theory. As an example, a severe decrease in tryptophan, an essential precursor to serotonin (a monoamine), can aggravate this illness in depressed individuals or families of depressed patients. Therefore, reducing serotonergic neurotransmission is important in treating depression. There is also a correlation between the risk of depression and a polymorphism in the 5-HTTLPR gene, which encodes serotonin receptors. Finally, evidence from mouse models indicates that adrenergic neurotransmission is reduced in depression due to a decrease in the size of locus circles, a decrease in tyrosine hydroxylase activity, and an increase in the density of alpha-2 adrenergic receptors.
In healthy people, however, low serotonin does not cause depression. Additionally, antidepressants rapidly increase monoamine levels, but it takes weeks to see their effects, and there are unusual antidepressants that impact treatment of this illness without targeting it directly.
There are also immune system abnormalities present in depression, including increased cytokines involved in the production of pathological behavior. The efficacy of nonsteroidal anti-inflammatory drugs (NSAIDs) and cytokine inhibitors in the treatment of depression, as well as the normalization of cytokine levels after successful treatment, suggest the presence of immune system abnormalities in the development of depression.
In light of the relationship between CRHR1 and depression, and the positive results of the dexamethasone suppression test (DST) in depressed patients, it has also been suggested that HPA-based abnormalities play a role in depression. Cortisol secretion increases in some patients with depression because of a dysfunction in the HPA axis. Glucocorticoids lower serum cortisol, so it makes sense that in depression, if cortisol levels are elevated, dexamethasone may not be able to lower them as much as usual, as indicated by the DST test. In any case, this anomaly is not sufficient as a diagnostic tool, since the test’s sensitivity is only 44%.
Brain imaging findings have also led to theories. A proposed model is the cortical, limbic model which describes the hyperactivity of the abdominal paralympic regions and the inactivity of the frontal regulatory regions. Another model is the cortico-striatal model, which suggests that depression is caused by abnormalities in the anterior cortex that regulate striated and subcortical structures. An alternative model proposes that emotional bias and depression are caused by the inactivation of brain structures that identify negative stimuli and inactivate cortical regulatory structures.
Diagnosis of depression :
A trained general practitioner, psychologist, or psychiatrist will examine a person’s current condition, life history, symptoms, and family history to determine the diagnosis. A clinical goal is to identify biological, psychological, and social factors that may affect a person’s mood. Alcohol and drug use are also taken into account by the evaluator. Assessments include examining the individual’s mental state, current mood, and intellectual content, especially in terms of pessimism or frustration, self-harm or suicide, and lack of positive thoughts.
Mental health services are scarce in rural areas, so primary care physicians are primarily responsible for diagnosing and treating this problem. This is more common in developing countries. Primary care physicians and other non-psychiatrists find it more difficult to diagnose and treat depression than psychiatrists. This is due to the illness’s physical symptoms and to the various barriers between the patient and the treatment system. According to a recent review study, non-psychiatrists are not diagnosing two-thirds of cases of depression.
A mental health examination may include the use of a rating scale, such as the Hamilton Rating Scale for Depression, the Beck Depression Inventory, or the Revised Suicide Behavior Questionnaire.
Only a score based on a scale can diagnose depression, but it does provide a measure of its severity. In such cases, a person whose score exceeds a threshold should be evaluated further for the final diagnosis of depression. Different scales are used for this.
To rule out other causes of the major depressive disorder, your doctor will perform a medical examination and selective tests. Tests include measuring thyroid-stimulating hormone and thyroxine to rule out hypothyroidism; measuring basal electrolytes and blood calcium to rule out metabolic disorders; and testing for systemic infections and chronic diseases.
There is also the possibility of adverse emotional reactions to some medications or alcohol abuse. A testosterone level may also be measured to diagnose hypogonadism, a cause of this illness in men. Decreased levels of vitamin D have also been associated with an increased risk of depression. Vitamin D levels can also be measured.
People with mental cognitive complaints often have depression, but they can also be signs of another illness, such as Alzheimer’s. Cognitive tests and brain imaging can help differentiate depression from dementia.
A CT scan of the brain can also assess the risk of brain damage in people with symptoms of psychosis, who develop symptoms quickly, or who have some unusual symptoms.
Depression cannot be confirmed by biological tests; biomarkers have been studied. Brain-derived neurogenic factors and several fMRI techniques are among these markers.
DSM and ICD criteria:

Diagnoses of depressive disorders are based on the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association and the International Statistical Classification of Diseases (ICD) of the World Health Organization.In Europe, the second classification system is commonly used, whereas in the United States and many countries outside of Europe, the first system is used.
The ICD-10 defines three common symptoms of depression (depressed mood, anhedonia, and low energy), two of which are essential for diagnosing the condition. According to the DSM-5, depression is characterized by two main symptoms: decreased mood and loss of interest and enjoyment in activities. In order to interfere with a person’s functioning, these symptoms, as well as a few others, should be present for two weeks at a time. In the DSM-5, major depressive disorder is classified as a mood disorder. One or more episodes of major recurrent illness are required for diagnosis. Both the episode itself and the period of the disorder are described by descriptors.
When the onset of a depressive episode does not meet the criteria for a primary depressive episode, an unspecified depressive disorder is diagnosed. ICD-10 does not use the term major depressive disorder but uses the same criteria to diagnose episodes of this illness (mild, moderate, or severe). The term recurrent is also added to the diagnosis if multiple episodes occur frequently and without manic intervals between episodes of depression.
Major Depression :
A major depressive episode consists of a depressed mood lasting at least two weeks. Isolated or recurrent episodes may be mild, moderate, or severe. Psychotic depression is automatically rated as severe when it has the characteristics of psychosis. The patient will be diagnosed with bipolar disorder if they experience mania.

Often, these criteria are criticized for ignoring other aspects of life in which this illness can occur. There is also little empirical support for the DSM-IV threshold.
Rejection causes of this illness include a range of related diagnoses, including mood disorders, including transient recurrent depressive episodes and mild depressive disorders with only few significant symptoms. Low mood caused by a psychological reaction to an identifiable event or stressor is accompanied by depressive mood.
New depressive disorders have been added to the DSM-5: Disruptive Mood Disorder, which is characterized by significant childhood irritability and mood disorders, Premenstrual Disorder, which causes anxiety, depression, or irritability in the weeks prior to menstruation.
Depression subsets:
Additionally to the duration, severity, and presence of psychotic features, the DSM-5 classification system defines six other subgroups of significant depression:
Loss of pleasure in most or all activities, a depressed mood stronger than grief, waking up in the morning with worsening symptoms, slowing down, slowing down, and slowing down, excessive weight or guilt are all symptoms of depressive melancholy.
2. The symptoms of atypical depression include mood responsiveness (paradoxical anhedonia) and positivism, significant weight gain or increased appetite, excessive sleep or insomnia, and heavy limbs (lead paralysis) as a result of hypersensitivity.

3. A catatonic depression is a severe form of major depression that includes impaired motor behaviors and other symptoms. Generally, the person is silent, almost confused, and exhibits immobility or aimless and strange movements. Catatonic symptoms may also be seen in schizophrenia or in episodes of mania and malignant neuroleptic syndrome.
4. An anxiety disorder associated with depression has been added to the DSM-V to emphasize the association between depression and anxiety, and the suicide risk among depressed people with anxiety.

5. Childbirth-related depression is a severe, persistent, and sometimes debilitating depression that some women experience after giving birth to a child. DSM-IV-TR used the term postpartum depression, but it was changed to depression with peripartum onset to include cases of depression during pregnancy. First-time mothers are about 10% to 15% more likely to suffer from postpartum depression. It can last up to three months. Some researchers believe that this depression is not unique to women and can also affect men after birth.
6. A type of depression in which episodes of depression appear in the fall or winter and disappear in the spring is known as Seasonal Affective Disorder (SAD). A diagnosis is made when at least two episodes occur in the colder months of two years or more and no episodes occur in other periods.
Other possible diagnoses include mood swings, depressive mood disorder, and bipolar disorder. A person with mood swings experiences a low mood daily for at least two years. These symptoms are not as severe as those of major depression. Yet, people with mood disorders are susceptible to secondary episodes of major depression (sometimes referred to as major depression).
The depressive mood adjustment disorder manifests as a psychological response to an identifiable event or stressor. The resulting emotional or behavioral symptoms are significant, but do not qualify as major depressive episodes.
In bipolar disorder, depressive and manic states manifest intermittently. Depression is currently classified as a separate disorder, but there is much debate about it. There is a link between major depression and mild mania in people with both disorders.
Before diagnosing major depression, other disorders should be considered. Chronic fatigue syndrome, depression caused by physical illness, medication, and substance abuse are examples. A physical illness is defined as a mood disorder caused by a general medical condition. History, laboratory results, or physical examination are used to diagnose this condition. When depression is caused by drugs, drug abuse, or exposure to toxins, it is diagnosed as a specific mood disorder (formerly known as substance-induced mood disorder in DSM-IV-TR).

Treatments for depression :
Psychotherapy, medication, and electric shock therapy are the three most common treatments for depression. Psychotherapy is the most common treatment for people under the age of 18. According to the 2004 recommendations of the National Institutes of Health and Clinical Excellence, antidepressants should not be used to treat mild depression in the early stages due to the low risk-to-benefit ratio. Antidepressant therapy should be continued for at least six months to reduce the risk of recurrence. SSRIs are better tolerated than tricyclic antidepressants (TCAs).
In accordance with the American Psychiatric Association’s treatment guidelines, initial treatment should be tailored to the patient’s symptoms, co-occurring disorders, past treatment experiences, and preferences. Medication, psychotherapy, exercise, electroconvulsive therapy (ECT), magnetic resonance imaging (TMS), or phototherapy may be used.
Evidence suggests that collaborative care provided by a group of health care professionals is better than the usual care provided by a specialist. Treatment options are more limited in developing countries, as access to mental health, medication, and psychotherapy is often difficult. The development of mental health services is fragile in many countries; Depression is considered a phenomenon in the developed world, although there is evidence to the contrary, and depression is not thought to be a life-threatening illness.

- Lifestyle change
Exercise is recommended for the treatment of mild depression, as it has a moderate effect on its symptoms. the treatment of mild depression, as it has a moderate effect on its symptoms. treating mild depression because it has a moderate effect on its symptoms, but it also seems effective for treating major depression. This approach is equivalent to medication or psychotherapy for most people. It also seems to reduce depression among older people. As in observational studies, the effects of smoking cessation on depression were as significant as those of drugs. Diet and sleep may also play a role in depression, and intervention in these areas can help depressed patients.
The effects of waking up during the night were visible the next day, according to one study. This effect is usually temporary, and in addition to drowsiness, this method can also cause manic symptoms.

2. Consultation
Individual, group, or family psychotherapy is available. In 2015, a review study showed that cognitive-behavioral therapy (CBT) was as effective as antidepressants. For more chronic and complex forms of depression, a combination of medication and psychotherapy may be more effective. According to a 2014 Cochrane review, occupational interventions combined with clinical interventions can reduce the number of days of depression. Evidence suggests that psychological therapies, in addition to standard treatment, are effective short-term antidepressants for treating refractory depression.
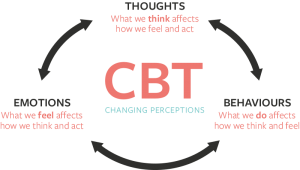
- Cognitive-behavioral therapy
There is the most research evidence for cognitive behavioral therapy (CBT) to treat depression in children and adolescents, and CBT and interpersonal psychotherapy (IPT) are the preferred treatments for adolescent depression. NICE recommends medication as well as psychological treatment, such as CBT, interpersonal therapy, or family therapy, for people under 18. People with depression have used several types of cognitive-behavioral therapy, including mindfulness, emotional and behavioral therapy, and mindfulness-based cognitive therapy. A mindfulness-based stress reduction program may reduce depressive symptoms.
Cognitive behavioral therapy is a common type of speech therapy that can be just as effective or even more effective than antidepressants in some cases. This type of therapy is typically used for mild to moderate depression. Even so, if the therapist is skilled enough, he can also use it to treat severe depression. CBT can be combined with other treatments, such as medication, in some instances. Thus, the therapist helps the patient identify their negative or incorrect thoughts and replace them with healthier and more realistic ones. An individual may feel worthless or believe that their life is terrible and getting worse. They may be severely tormented by their weaknesses and shortcomings. CBT informs the person that they have these thoughts in the beginning. It then teaches them how to replace those negative thoughts with positive ones. Changes in a person’s attitude can lead to changes in their behavior and reduce depressive symptoms. With CBT, he learns to say to himself, “This is not a useful idea; there are many rewards to trying.” I begin my struggle to get out of bed with CBT. Of course, to achieve that state of feeling good, it takes weeks and sometimes even months to attend these sessions.
CBT is the most widely accepted method of speech therapy. Some types of depression can be treated using this method as effectively as with antidepressants. It has been shown in some studies that people treated with CBT have a 50 percent higher chance of relapsing than those treated with medication alone.
When combined with medication, CBT may be more effective in treating depression, and the benefits may last longer. The majority of people treated with CBT for depression or anxiety continue to use their skills one year later.
Let’s say someone is taking medication for depression. Even if he or she is working with a CBT therapist, he or she should never stop taking the medication without consulting the prescribing physician. When someone abruptly stops taking their medication, it can lead to severe depression and other problems.
- Interpersonal psychotherapy to treat depression
It focuses on past and present social maps and interpersonal interactions for patients with depression. A therapist usually focuses on one or two areas of the patient’s life that seem to be the source of their problems during treatment. Conflict with friends, family, co-workers, grief over loss, and divorce and retirement changes are some of these areas. The aim of the IPT is not to delve into internal conflicts, but to help the patient find better ways to deal with problems.
There are two kinds of IPT. For short-term treatment of depression, the first type is used. The patient and therapist usually meet weekly for two to four months, and when the symptoms subside, the treatment is over. Maintenance therapy (IPT-M) is a long-term treatment that prevents or reduces future episodes of depression. Patients attend monthly meetings for two to three years.
Interpersonal therapy focuses on four primary problem areas. The therapist helps the patient to determine which area is most responsible for his or her depression, then directs the treatment to help the patient deal with the problem in that area. Interpersonal therapy recognizes four primary problem areas:
- Unresolved grief: In normal mourning, the person usually returns to normal within a few months. Unresolved grief is delayed and persists for a long time afterward, or is distorted grief in which a person may not feel emotional but experience other symptoms instead.
- Role conflicts: Role conflicts occur when the patient and the critical people in his or her life have different expectations about their relationship.
- Role change: When a person’s role in life changes, he or she may not know how to cope, and this change will be the source of his or her problems.
- Interpersonal conflicts: If the patient has problems establishing and maintaining quality relationships, this area may be of interest to the therapist.
5. Use of psychoanalysis in the treatment of depression
Psychoanalysis was founded by Sigmund Freud and focuses on conflicts in the subconscious mind. Psychoanalysis may be used to treat major depression.
A scanning psychotherapy session takes place once or twice a week and is of low intensity. Scanning psychotherapy aims to help patients fully explore their emotions, including those they may not be aware of. Psychotherapy helps people understand how unresolved issues and unconscious emotions affect their behavior and mood.
One of the three main types of psychotherapy used to treat depression is scanning therapy. The other two are cognitive behavioral therapy and interpersonal therapy. These methods differ by their focus. Both CBT and IPT aim to understand and modify a specific process or behavior. The focus in CBT is on how one thinks. CBT focuses on identifying and changing abnormal thinking patterns that determine how a person acts and feels. IPT focuses on identifying issues and problems in interpersonal relationships and finding solutions. CBT and IPT both have a time limit and are considered short-term treatments. This method focuses on learning new patterns rather than analyzing the causes of abnormal patterns.
In contrast, psychotherapy is based on Freud’s theories and methods of psychoanalysis. Psychology is based on the idea that a person’s subconscious mind and past experiences influence their behavior. A psychoanalyst examines a patient’s emotions intensively and open-ended over the course of several sessions per week. During the first session, we discover the patient’s emotions and those that he is unaware of.
A scanning psychotherapy session lasts about 50 minutes and usually takes place once a week. Patients are usually seated in a chair without seeing a therapist. In contrast to IPT and CBT, which involve formal, structured sessions, dynamic psychotherapy is typically open-ended and unstructured. The patient is encouraged to discuss freely what has happened to him or her or what is on his or her mind during dynamic psychotherapy. In doing so, the patient’s behavior and emotions are rooted in past experiences, and new emotions emerge. As a result, they will become more aware of how past experiences and the subconscious mind affect their daily lives. Scanning psychotherapy is not necessarily a short-term or limited treatment. Some treatment courses end after 16 to 20 weeks, while others may last for more than a year.
Psychotherapy involves exploring the full range of emotions a patient is experiencing. Therapists help their patients talk about their feelings, including conflicting feelings, distressing or threatening feelings, and unfamiliar feelings. One discovers that the ability to explain the cause of a problem does not necessarily translate into the ability to solve it. We attempt to cultivate the internal resources necessary for individuals to cope with and effectively manage those problems.
Apart from focusing on emotions, dynamic psychotherapy also recognizes and addresses a patient’s defense mechanisms, namely, the reactions and behaviors they use to avoid disturbing thoughts and feelings. People may, for example, try to suppress memories of unpleasant experiences or change the subject when talking about specific subjects. Alternatively, one may be late or not attend meetings that have reached very unpleasant topics or focus on external details instead of focusing on one’s role in an issue. During the sessions, patterns of thinking, emotions, and behavior will emerge in the patient. Often, these patterns are subtle, and the patient cannot recognize them.
During therapy, the therapist helps the patient recognize these patterns and understand how they affect their mood and reactions. Sometimes the discussion of patterns leads to a review of past experiences that are still relevant today. In scanning psychotherapy, emphasis is also placed on dynamic relationships, especially those between therapist and patient. A therapist can gain insight into how a patient reacts and interacts with others by observing their behavior in that relationship.
The majority of psychological problems arise from a person’s relationship with others and inability to meet their emotional needs. In scanning psychotherapy, the goal is to identify these problems and find ways to solve them or deal with them better. Psychodynamic therapy examines the imaginary dimension of a person’s life, including the psychological concepts behind imaginary scenes and the emotional content of dreams. The patient will discover everything in his mind because he is encouraged to speak freely.

Psychodynamic therapy’s primary goals are to gain more knowledge about one’s subconscious conflicts and self-awareness of one’s emotions and motivations. This insight is thought to be the mechanism by which symptoms are relieved. Also, dynamic psychotherapy aims to help the patient develop internal psychological resources and increase their capacity to deal with the psychological problems that cause them emotional pain and suffering. The person does this by dealing with subconsciously suppressed issues that affect his or her life or learn healthier ways to deal with them.
Until recently, it was thought that there was no evidence to support the effectiveness of dynamic psychotherapy as a treatment for depression. Part of the reason was that experimental research did not focus on scanning psychotherapy participants as participants in CBT and IPT. But over the past few decades, that situation has changed, and studies have emerged.
In early 2010, a report published in the journal American Psychologist reviewed data from existing dynamic psychotherapy and depression studies. The authors conclude that dynamic psychotherapy is at least as effective as other evidence-based therapies and that the benefits of this treatment appear to be more lasting.

- Antidepressants
Studies that have examined the effectiveness of antidepressants in treating people with acute, moderate, and mild depression have yielded conflicting results. More substantial evidence supports the usefulness of antidepressants in treating severe or chronic depression. One review found that SSRIs such as citalopram, paroxetine, and sertraline were more effective than placebo at reducing depression scores in primary and moderate major depression. There was evidence that such effects were also seen in mild depression.
A systematic review of Cochrane’s clinical trials of the amitriptyline tricyclic antidepressant shows that it is more effective than placebo. In 2014, the Food and Drug Administration conducted a systematic review of all antidepressant tests submitted to the agency between 1985 and 2011. The authors concluded that maintenance therapy reduced recurrence risk by up to 52% compared with placebo.
The amount of medication should be adjusted, and different groups of antidepressants are used if necessary. The response rate to the first antidepressant used is 50 to 75%, and it takes at least 6 to 8 weeks to observe the effect of the drug.
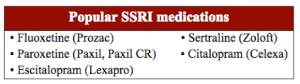
Antidepressant medications usually last 4 to 6 months after recovery, and it is sometimes recommended that they be continued for up to a year. People with chronic depression may need to take medication indefinitely to avoid recurrence. SSRIs are usually the first drugs to be prescribed because of their relatively mild side effects and the fact that high doses are less toxic than other antidepressants.
SSRIs not affected by SSRIs can take another antidepressant, which can improve about 50% of cases. Another option is to use the unusual antidepressant bupropion. Venlafaxine is also an antidepressant with different mechanisms of action that may be more effective than SSRIs. However, venlafaxine is not recommended as a first-line drug in some countries, such as the United Kingdom, due to its potential risks and adverse effects on children.

Some studies have recommended the use of the antidepressant fluoxetine in children. However, the drug is not recommended for children with mild illnesses.
Antidepressants can lower blood sodium levels, although this has been reported more often in SSRIs. SSRIs can cause insomnia or worsen existing insomnia so that the unusual sedative antidepressant mirtazapine can be used.
Irreversible monoamine oxidase inhibitors are an older group of antidepressants that are less well-known because of their potential interactions with diet and medication.
In adults, it is not clear whether this group of drugs affects the risk of suicide. In 2007, SSRIs and other antidepressants were issued a black box warning in the United States to increase the risk of suicide in patients younger than 24 years. The Japanese Ministry of Health issued such precautionary warnings.
7.Three-ring and four-ring antidepressants
Tricyclic and quadruple antidepressants are antidepressants that affect brain chemicals. These antidepressants, also called ring antidepressants, were one of the first drugs developed to treat depression. They are effective but have generally been replaced by antidepressants that cause fewer side effects.
However, ringworm antidepressants may be a good option for some people. In some cases, they can treat depression when other therapies are ineffective. Cyclic antidepressants are designed in three cycles or four cycles. These numbers refer to the number of rings in their chemical structure.
Ring antidepressants treat depression by acting on neurotransmitters used to communicate between brain cells. These drugs inhibit the neurotransmitters’ reabsorption of serotonin and norepinephrine and increase these two neurotransmitters’ levels in the brain. Ring antidepressants also affect other chemical messengers and can therefore cause a variety of side effects. The Food and Drug Administration has approved the following three-pronged antidepressants for the treatment of depression:
- Amitriptyline
- Amoxapine
- Desipramine
- Doxepin
- Imipramine
- Nortriptyline
- Protriptyline
- Trimipramine
Maprotiline, a four-cycle antidepressant, has also received FDA approval for the treatment of depression. Cyclic antidepressants are sometimes used to treat problems other than depression, such as anxiety disorders or nerve pain.
Due to the different routes of action of antidepressants, the side effects also vary somewhat from drug to drug. Some side effects may go away over time, while others may cause another medicine to be prescribed. Side effects may also depend on the amount of medication, and higher doses may cause more side effects. Some possible side effects include:
- Blurred vision
- Constipation
- Dry mouth
- Drowsiness
- Hypotension when changing position from sitting to standing
- Urinary retention
- Increased appetite and weight gain
- Weight Loss
- Excessive sweating
- Tremor
- Sexual problems in the field of erection, orgasm, or decreased sexual desire

In general, we can say:
- Amitriptyline, doxepin, imipramine, and trimipramine are more likely to cause drowsiness than other tricyclic antidepressants. Taking these medications at bedtime may help solve this problem.
- Amitriptyline, doxepin, and imipramine are more likely to cause weight gain than other tricyclic antidepressants.
- Side effects of nortriptyline and desipramine appear to be easier to tolerate than other tricyclic antidepressants.
- Some tricyclic antidepressants may cause safety-related side effects:
- Loss of direction or confusion, especially in the elderly when the dose of the drug is very high
- Increased heart rate or irregular heartbeat
- More seizures occur in people who have seizures.
Your doctor may order blood tests to determine the best amount of medicine. Some of the side effects and benefits of tricyclic antidepressants depend on the amount of medication. Overuse of antidepressants can be dangerous. Ringworm antidepressants can cause problems in people with specific health problems. For example, suppose a person has glaucoma, an enlarged prostate, heart problems, diabetes, liver disease, or a history of seizures. In that case, they should talk to their doctor about whether this antidepressant is right.
- Stop the antidepressant treatment regimen:
Ring antidepressants are not considered addictive drugs. However, abrupt discontinuation of treatment or postponement of several uses can cause pseudo-withdrawal symptoms. Symptoms may vary depending on how the medicine works. This condition is sometimes referred to as withdrawal syndrome. Consult your doctor for a gradual and safe reduction in the amount of medication.

Symptoms of quasi-withdrawal may include:
- Confusion, irritability, or anxiety
- nausea
- Transpiration
- Influenza-like symptoms such as chills and muscle aches
- insomnia
- Lethargy
- Headache
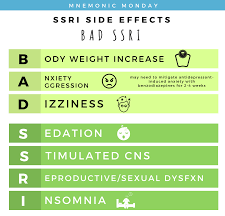
9.Selective serotonin reuptake inhibitors
Selective serotonin reuptake inhibitors (SSRIs) are the most common prescription antidepressants. They can reduce the symptoms of moderate to severe depression and are relatively safe, and usually have fewer side effects than other antidepressants.
SSRIs reduce depression by increasing serotonin levels in the brain. Serotonin is a neurotransmitter that transmits signals between brain cells. This group of antidepressants inhibits the reuptake of serotonin in the brain and increases access to serotonin. SSRIs are called “selective” because they only affect serotonin. SSRIs are also used to treat conditions other than depression, such as anxiety disorders.

Approved SSRIs for the treatment of depression: The Food and Drug Administration has approved these SSRIs for the treatment of depression:
- Citalopram
- Sclitopam
- Fluoxetine
- Paroxetine
- Sertraline
- Vilazodone
Fluvoxamine is an SSRI approved by the FDA to treat obsessive-compulsive disorder and is sometimes used to treat depression.
Possible side effects:
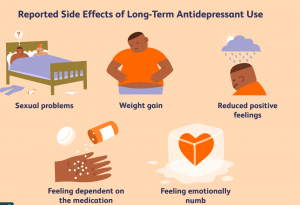
All SSRIs have the same mechanism of action and can cause the same side effects. However, some people may not experience any of these side effects. Many side effects may go away within the first few weeks of treatment, while some may cause the patient to see a doctor and prescribe another medication. Possible side effects of SSRIs include:
- Drowsiness
- nausea
- Dry mouth
- insomnia
- Diarrhea
- Burning, confusion, or restlessness
- Vertigo
- Sexual problems such as decreased libido or orgasm or erectile dysfunction
- Headache
- Blurred vision
Taking these medications with food may reduce the risk of nausea. Also, if the drug does not interfere with sleep, it can reduce nausea during sleep. Which antidepressant is right for a person depends on factors such as their symptoms and other health problems.
SSRIs are generally safe for most people, but in some cases, they can cause problems. For example, high doses of citalopram can cause dangerous abnormal heart rhythms. Other issues that should be considered before taking this type of medication are:
- Drug Interactions: Before taking an antidepressant, consult your doctor about other medications. Some antidepressants can cause dangerous reactions when combined with certain herbal medicines or supplements.
- Serotonin Syndrome: Rarely can an antidepressant drug cause high serotonin levels to build up in the body. Serotonin Syndrome often occurs when two drugs that increase serotonin levels are combined. These include other antidepressants, specific and headache medications, and St. John’s wort herbal supplements. Signs and symptoms of serotonin syndrome include anxiety, aggression, transpiration, confusion, tremors, restlessness, lack of coordination, and increased heart rate. If any of these symptoms occur, it is necessary to see a doctor.
- Antidepressants and pregnancy: The patient should talk to their doctor about the risks and benefits of using a particular antidepressant. Some antidepressants may harm the fetus and baby if used during pregnancy or lactation.
- Suicide risk and antidepressants: Most antidepressants are generally safe, but the FDA requires all antidepressants to have a black box warning. In some substances, children, adolescents, and young people may experience suicidal thoughts or behaviors while taking antidepressants, especially in the first few weeks after starting or when the dose changes. Anyone taking an antidepressant should be monitored for worsening symptoms or abnormal behaviors. If a person develops suicidal thoughts while taking these drugs, it is necessary to see a doctor. However, it should be noted that antidepressants generally reduce the risk of suicide in the long run by improving mood.
Discontinuation of SSRI treatment :
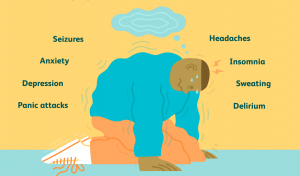
SSRIs are not considered addictive. However, abrupt discontinuation of antidepressants or failure to take medication several times can lead to suspected withdrawal symptoms. This is sometimes called “withdrawal syndrome.” To reduce the dose of the drug should follow the advice of your doctor. Symptoms of suspicion may include:
- The feeling of general malaise
- nausea
- Vertigo
- Lethargy
- Flu-like symptoms
Other drugs :
There is evidence that fish oil supplements containing omega-3 fatty acids, which have high levels of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are effective in treating rather than preventing major depression. However, a Cochrane review found insufficient evidence for the effect of omega-3 fatty acids on depression.
There is little evidence that vitamin D supplementation effectively reduces depressive symptoms in people with vitamin D deficiency. There is also preliminary evidence that COX-2 inhibitors such as celecoxib have a beneficial effect on major depression. Lithium also appears to effectively reduce the risk of suicide in people with bipolar disorder and unipolar depression to the general population level. Of course, there is a fine line between practical and safe lithium, so care must be taken to use this element. Low doses of thyroid hormone may also be added to existing medications to treat the symptoms of chronic depression in people who have taken several courses of medication. Stimulants such as amphetamines and modafinil may also be useful in the short term or as adjunctive therapy. Folate supplements may also play a role in managing depression. There is also empirical evidence regarding the benefits of using testosterone in males.
Find the right antidepressant :
Different people may not have the same reaction to a similar antidepressant. For example, a particular drug may work for one person or have no effect on another, or side effects may occur only in some people. Hereditary traits play a role in how antidepressants affect an individual. In some cases, specific blood tests may explain how a person responds to an antidepressant. However, variables other than genetics can also play a role in a person’s response to these drugs. When choosing an antidepressant, your doctor will consider your patient’s symptoms, health problems, and other medications, as well as your history. It usually takes weeks for an antidepressant to be fully effective. You may have to change the type or amount of medication to find the right type and amount of medication recommended by your doctor.
Electroshock treatment:
Electroshock therapy (ECT) is a standard psychiatric treatment in which patients are electrically induced seizures to relieve mental illness. This method is used as a last resort option to treat major depressive disorder and patient satisfaction. An ECT cycle is effective in about 50% of people with refractory major depressive disorder (bipolar or unipolar), but about half of those who respond to this treatment and return to the disease within the next 12 months. Apart from this method’s effects on the brain, this method’s side effects are like general anesthesia, and the person may be confused and have a poor memory for a short time after treatment. A typical ECT course involves using the shock several times (usually two or three times a week) until the patient no longer shows symptoms.
Electroshock therapies differ in several ways: the electrodes’ location, the frequency used for the treatment, and the electrical waveform of the stimulus. These methods differ in terms of possible side effects and terms of symptom relief. After this treatment, medication is usually continued, and some patients receive ECT maintenance treatment. It seems that the short-term effects of this method are due to the anticonvulsant effect on the frontal lobes and its long-term effects are due to neurotrophic effects on the temporal lobe.
Magnetic stimulation of the brain through the skull
Cranial magnetic stimulation (TMS), or deep magnetic stimulation, is a non-invasive way to stimulate small brain areas. In 2008, the TMS method was approved by the FDA as the treatment for major refractory depression, and in 2014, evidence was obtained that it was effective. The American Psychiatric Association, the Network for Anxiety and Mood Disorders in Canada, and the Royal College of Psychiatrists in Australia and New Zealand have endorsed TMS to treat major refractory depression.
Other treatments
Phototherapy reduces the severity of depressive symptoms and has benefits for seasonal affective disorder and non-seasonal depression, and has an effect similar to regular antidepressants.
Prognosis of depression :
Significant episodes of depression, whether treated or not, usually resolve over time (but recurrence is possible). Studies show that outpatients who have not yet been treated have a 10 to 15 percent reduction in symptoms after a few months, and about 20 percent no longer meet the full criteria for depressive disorder. It is estimated that the middle of an episode is 23 weeks, and the highest recovery rate occurs in the first trimester. Studies have shown that 80% of people who experience a significant episode of depression once in their lifetime will experience at least one or more episodes in their lifetime (average four episodes in their lifetime).
If the symptoms are not entirely treated, they are more likely to come back or become chronic. Current guidelines recommend that antidepressants continue to be used for six months after recovery to prevent a recurrence. People who experience recurrent episodes of depression need long-term treatment to prevent more severe and long-term depression.
Depressed people have a lower life expectancy than non-depressed people because depressed patients are at risk of suicide. However, they also have a higher risk of dying from other factors and are more susceptible to heart disease diseases.
Up to 60% of people who die from suicide have a mood disorder such as major depression. The risk is exceptionally high when the person experiences significant frustration or has depression and borderline personality disorder.
Depression is often associated with unemployment and poverty. Major depression is currently the leading cause of illness in North America and other high-income countries and is the fourth leading cause worldwide. According to the World Health Organization, by 2030, the disease will be the second leading cause of disease worldwide after HIV. Delay or failure to seek treatment after relapse and the inability of health professionals to provide treatment are obstacles to reducing disability caused by the disease.
Epidemiology of Depression:
Major depressive disorder affected approximately 216 million people in 2015 (3% of the world’s population). In most countries, the number of people who get the disease in their lifetime is 8 to 18 percent. In North America, the probability of having a significant episode of depression over an annual period is 3 to 5 percent for men and 8 to 10 percent for women.
Prevalence of depression:
The first episode of depression is more likely to occur between the ages of 30 and 40, and there is a second, smaller peak between the ages of 50 and 60. The risk of major depression increases during the first year after delivery, despite neurological problems such as stroke, Parkinson’s disease, or multiple sclerosis. The prevalence of this disease is after cardiovascular diseases.
Depressive disorders are more common in urban communities than in rural communities, and the prevalence of this disease is higher in people with socioeconomic problems such as lack of housing.
Aging and depression :
Depression is especially prevalent among people over the age of 65, and its prevalence increases with age. Also, the risk of developing depression increases as a person becomes weaker. Depression is one of the most critical factors affecting the quality of life in adults and the elderly.
Both the symptoms and the treatment differ among the elderly and those in the community. Like many other diseases, the classic symptoms of the disease may not be seen in the elderly. Because older people often have other illnesses and medications simultaneously, it is more challenging to diagnose and treat depression.
Depression in old age :

Different treatments are used in this group of people. The results of studies have shown that the effect of SSRIs on the elderly is not satisfactory. On the other hand, although drugs such as deluxe (a serotonin reuptake inhibitor) have been significant, side effects such as dizziness, dry mouth, diarrhea, and constipation are complicated to tolerate in the elderly prevent the drug from being prescribed.
Research related to depression :
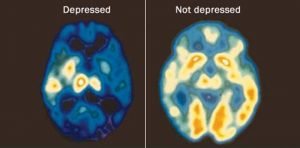
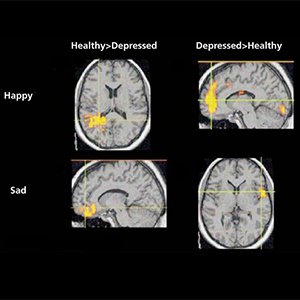
MIR scans of depressed patients show differences in people’s brain structure with depression compared to non-depressed people. According to a meta-analytic study, depressed patients had increased volume in the lateral ventricles and adrenal glands and smaller volumes in the basal ganglia, thalamus, hippocampus, and frontal lobe (including the cortex and right gyrus) compared with controls. In the brains of people with this disorder in old age, there are signs of congestion on brain scans, which has led to the theory of “vascular depression.”
Experiments are investigating the effects of botulinum toxin on depression. The idea is that this drug prevents frowning on the patient’s face, and this prevents negative facial feedback. However, the results of 2015 showed that the positive effects observed could be due to placebo effects.
In 2018, the US Food and Drug Administration approved a Phase 2 study of psilocybin to treat refractory depression.