Everything you need to know about blood clots
Blood clots are like blood clots that, when formed in response to injury or cutting and blockage of a damaged blood vessel, help prevent bleeding. A small number of blood clots flow in the arteries and do not heal naturally, and these may need medical attention, especially if they are in your legs or vital places such as the lungs and brain.
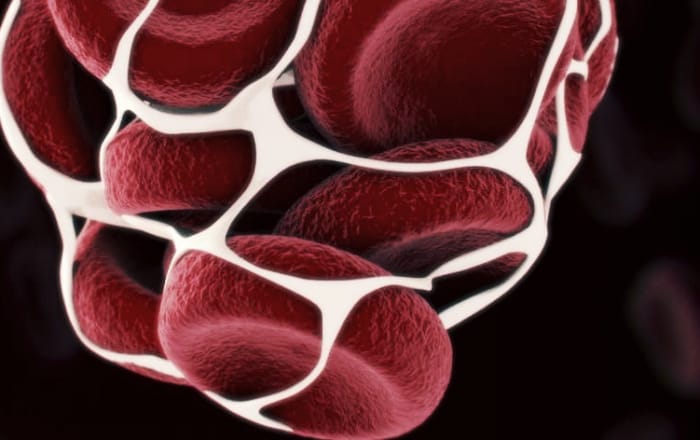
Blood clots form when blood clots and plasma proteins form a semi-solid mass. This process may be stimulated by lesions and sometimes may occur inside blood vessels and cause damage. After this type of clot, they can spread to other parts of your body and cause damage.

What causes blood clots?
Causes and conditions of blood clotting as well as serious diseases associated with blood clotting:
- Antiphospholipid syndrome
- Atherosclerosis / Atherosclerosis
- Certain medications, such as birth control pills and hormonal medications
- Deep vein thrombosis (DVT)
- Family history of blood clots
- Cardiac arrhythmia (heart rhythm problems)
- heart attack
- Heart failure
- Obesity
- Peripheral artery disease
- Pulmonary vera
- Pregnancy
- Sit or rest for a long time
- Pulmonary embolism (blood clots in a pulmonary artery)
- smoking
- Stroke
- Surgery
When should you see a doctor for a blood clot?
- If you experience these, seek medical attention:
- Cough with bloody sputum
- Fast heart rate
- Series style
- Difficult or painful breathing
- Chest pain or tightness
- Pain in the shoulder, arm, back, and jaw
- Sudden weakness or numbness of the face, hands, or feet
- Sudden difficulty in speaking or understanding speech
- Sudden changes in vision
To reduce the risk of blood clots, try these tips:
- Avoid sitting for long periods.
- If you travel by plane, take alternate walks in the hallway.
- For long trips, drive and walk a lot.
- Move.
- It is better to wake up and move as soon as possible after surgery or bed rest.
- Drink plenty of fluids throughout the day. Dehydration can help cause blood clots.
- Change your lifestyle. Weight loss, high blood pressure, smoking cessation, and regular exercise are good for everyone.
Blood coagulation process:
- These are the protein factors in the blood that control bleeding. When a blood vessel is damaged, the walls of the blood vessels constrict to restrict blood flow to the affected area.
- Small blood cells called platelets then attach to the affected area and spread along the surface of the blood vessel to stop bleeding.
- At the same time, chemical signals are emitted from small sacs inside the platelets that absorb other cells into the area and bind them together to form something called a platelet plug.
- Different coagulation factors work in a series of complex chemical reactions (known as coagulation cascades) to form fibrin clots at the surface of these active platelets. This clot acts like a net to prevent bleeding.
- Coagulation factors circulate passively in the blood. When a blood vessel is damaged, the coagulation chain begins, and each coagulation factor is activated to form a blood clot. Roman numerals identified coagulation factors.
How blood clots form:
The coagulation cascade is a complex chemical process that uses many different proteins in the blood.
This changes the process of blood clotting from liquid to solid at the site of injury. How this process works:
Vascular injury:
A small tear in the vessel wall (for example, an incision in the skin or an internal injury) causes bleeding.
Artery:
To control bleeding, the blood vessel narrows and restricts blood flow through the ship.
Platelet plug:
In response to the injury, tiny blood cells called platelets are activated. The platelets attach and attach to the wound site to form a plug. This protein factor (VWF) helps connect platelets and blood vessel walls.
Fibrin clots:
Next, coagulation factor proteins stimulate the production of fibrin, a strong substance and a similar filament that forms the fibrin clot, which is a fibrin clot that remains strong and stable. Over the next few days, the chunk strengthens, and the wound heals after the vessel wall heals.
The life cycle of a normal blood clot depends on a series of chemical reactions.
- Platelets of the plug:
When a blood vessel is damaged, small pieces of blood called platelets are released into your bloodstream. They stick to the area’s walls and form a plug that fills the broken part to prevent blood leakage. Once activated, they release chemicals to absorb platelets and other cells and begin the next step.
- The clot grows:
The proteins in your blood are called coagulation factors, which indicate a rapid chain reaction to each other. A soluble substance in your blood leads to long fibrin strands combined with platelets to form a network that traps even more platelets and cells. This clot becomes much harder and more stable.
- Reactions prevent it from growing:
Other proteins neutralize excess coagulation factor proteins, so the clot does not go beyond that.
- The body slowly breaks it:
Once the damaged tissue has healed, you no longer need to clot. The hard fibers of fibrin dissolve, and your blood returns the platelets and cells of this clot. The process of blood clotting is complex and causes many reactions. However, these reactions can be summarized in three steps.
A set called the prothrombin activator is produced by a long chain of chemical reactions. The prothrombin activator converts a blood protein called prothrombin into another protein called thrombin.
Thrombin converts soluble fibrinogen into an insoluble protein called fibrin. Fibrin is in the form of solid fibers that are located on the wound. This network traps platelets and other blood cells and forms blood clots.
Prothrombin and fibrinogen are always present in the blood but are not activated until a prothrombin activator is damaged. Blood coagulation occurs in a multi-step process called a coagulation cascade. This process involves many different proteins.
A waterfall is a chain reaction that leads from one stage to another. In general, each step produces a new protein that acts as an enzyme or catalyst for the next step.

Coagulation waterfalls are often divided into three paths:
External path, internal way, and common path.
The external pathway is stimulated by a chemical called tissue, which is released by damaged cells. This pathway is “external” because a factor outside the blood vessels initiates it. Also known as the tissue factor pathway.
The internal pathway is stimulated by the entry of blood into the collagen fibers in the broken wall of blood vessels. Eventually, both paths produce a prothrombin activator. The prothrombin activator stimulates the common pathway that prothrombin continues through the conversion of fibrinogen to fibrin.
Processes and stages of blood clotting in the body:
Homeostasis occurs when there is blood outside the body or blood vessels. This is the body’s instinctive reaction to stop bleeding and blood loss. During homeostasis, three stages occur rapidly, respectively. Vascular seizures are the first response to blood vessels that allow less blood to be lost.
In the second stage of platelet plug formation, the platelets stick together and form a temporary barrier to cover the rupture of the vessel wall. The third and final stage is blood clotting and coagulation.
It strengthens fibrin coagulation, which acts as a “molecular adhesive.” Platelets are a major factor in the process of chemical coagulation. They allow the formation of “platelet plugs” that form almost after a blood vessel ruptures. It takes about sixty seconds for the first fibrin fibers to separate from the wound.
Homeostasis is maintained in the body through three mechanisms:
1- Damaged blood vessels constrict
Vascular seizures are the first response to injury. Damaged arteries constrict, restricting blood flow to the area and reducing blood loss. This response is triggered by direct damage to vascular smooth muscle, chemicals released by endothelial cells, and platelets. Is stimulated
As the damage increases, the seizure response becomes more effective. Vascular seizures are much more effective in smaller vessels.
2- Platelet plug formation
Platelets damage the endothelium, causing platelet plugging (primary homeostasis) and then cannulation. This process is set up via the Internet. Platelets are one of the main factors in the process of chemical coagulation. The second step in their sequence (aggregation) is to form a plug that temporarily seals the gap in the ship’s wall.
Platelets attach to the collagen fibers of the wound and go up and down. Then chemical peaks release adenosine diphosphate (ADP), serotonin (ADP), and serotonin 2.
These chemicals are released, causing platelets to stick to the area and remove their contents, increasing vascular spasm. As more chemicals are released, platelets release them and release their chemicals. Platelets alone are responsible for preventing bleeding and tearing of our skin.
The second stage of homeostasis involves platelets that travel through the blood. When platelets are exposed to an area or lesion, they form a platelet plug. After the platelet plug is formed, coagulation factors begin to form blood clots. When this happens, coagulation factors start to develop a collagen fiber called fibrin.
When fibrinogen is converted to fibrin and added to platelets (secondary homeostasis), blood clots form.
Coagulation: The third and final step in this rapid response is platelet plug amplification. Blood coagulation uses fibrin fibers that act as adhesives for sticky platelets. As the fibrin network begins to form in the bloodstream, it is converted from a fluid to a fluid through coagulation factors and coagulants. The coagulation process is useful in closing and maintaining platelet branches in large wounds.
Prothrombin clotting also plays an important role in the coagulation process because it causes clot formation or clotting. This final stage forces the blood cells and platelets to stay in the affected area.
Although this is often a good step for wound healing, if the clot separates from the vessel wall and passes through the circulatory system, it can lead to stroke, heart attack, or pulmonary embolism. However, without this healing process, wounds are not possible.
Blood clotting disorders:
The body’s homeostasis system must be adjusted for proper functioning.
If the blood does not clot enough, it may be due to a bleeding disorder. Excessive clotting can cause problems. Thrombosis, in which blood clots form abnormally, can be potentially dangerous, where the blood clots become blocked and subsequently form in a vein or artery.
Homeostasis occurs for a variety of reasons. It may be due to a defect in platelets or hereditary coagulation factors. Several diseases are also available.


