How to detect stomach cancer early
Stomach cancer, also known as gastric cancer, is a type of cancer that originates in the lining of the stomach. It is a significant health concern worldwide, with an estimated 1 million new cases and 783,000 deaths each year. Stomach cancer often develops slowly over many years and can go undetected in its early stages, making it difficult to treat effectively.
There are several risk factors associated with stomach cancer, including a family history of the disease, a diet high in salted, smoked, or pickled foods, and certain medical conditions such as Helicobacter pylori infection and chronic gastritis. Other factors that may increase the risk of developing stomach cancer include smoking, alcohol consumption, and obesity.
Symptoms of stomach cancer can be non-specific and may include nausea, loss of appetite, abdominal pain, and unintentional weight loss. As the cancer progresses, more severe symptoms such as blood in the stool, vomiting, and difficulty swallowing may occur.
Early detection is crucial for successful treatment of stomach cancer. Treatment options may include surgery, chemotherapy, and radiation therapy. Additionally, lifestyle changes such as adopting a healthy diet and quitting smoking may help to reduce the risk of developing stomach cancer.
In this article, we will explore the causes, risk factors, symptoms, and treatment options for stomach cancer, as well as ways to reduce your risk of developing this disease.
I. Introduction
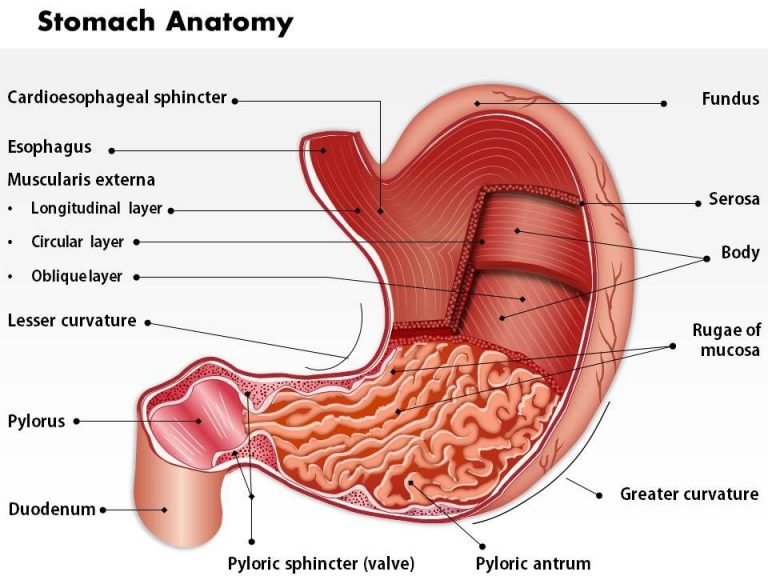
A. Definition of gastric cancer:
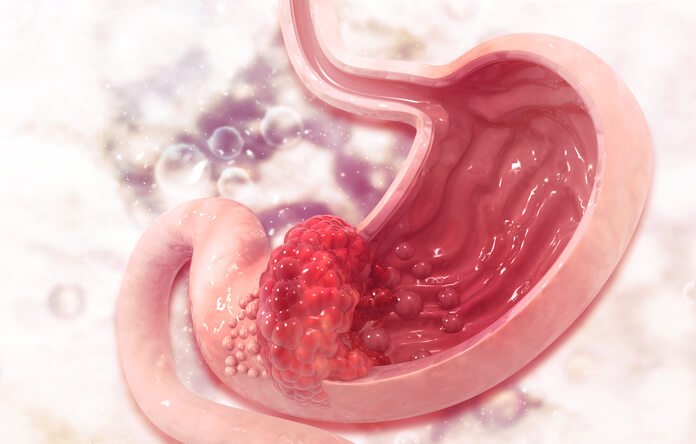
Gastric cancer, also known as stomach cancer, is a malignant tumor that arises from the cells lining the stomach. This type of cancer can occur in any part of the stomach and can spread to nearby organs or metastasize to distant parts of the body through the bloodstream or lymphatic system. Gastric cancer can be classified into various histological types, with the most common being adenocarcinoma, which accounts for about 90% of all cases. Other types include lymphoma, gastrointestinal stromal tumors (GIST), and neuroendocrine tumors.
B. Epidemiology and global prevalence:
Gastric cancer is the fifth most common cancer worldwide and the third leading cause of cancer-related deaths. The incidence of gastric cancer varies significantly by region, with the highest rates found in Eastern Asia, particularly in countries like Japan, China, and South Korea. Other areas with elevated incidence rates include Eastern Europe, Central and South America, and parts of Africa. The incidence of gastric cancer has been declining in recent decades, partly due to improved living conditions and better access to healthcare. However, it still poses a significant health burden, especially in developing countries.
C. Importance of early detection and treatment:
Early detection and timely treatment of gastric cancer are crucial for improving patient outcomes. When detected at an early stage, gastric cancer has a higher chance of being treated successfully, and the overall survival rate can be significantly improved. Unfortunately, gastric cancer is often asymptomatic or presents with nonspecific symptoms in its early stages, making it difficult to diagnose. As a result, many patients are diagnosed at advanced stages when the cancer has spread, and treatment options become limited. Increasing awareness about gastric cancer, its risk factors, and symptoms can help in promoting early detection and timely intervention, ultimately improving the prognosis for patients affected by this disease.
II. Causes and Risk Factors
A. Genetic factors:
There is evidence that genetic factors play a role in the development of gastric cancer. While most cases of gastric cancer are sporadic, around 1-3% of cases are hereditary and can be attributed to specific genetic mutations. Some of the known hereditary syndromes associated with an increased risk of gastric cancer include hereditary diffuse gastric cancer (HDGC), caused by mutations in the CDH1 gene, and Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC). Additionally, there is evidence that certain common genetic variations, known as single nucleotide polymorphisms (SNPs), may be associated with a higher risk of gastric cancer.
B. Helicobacter pylori infection:
H. pylori infection is the most significant risk factor for gastric cancer. This bacterium colonizes the stomach lining and can cause chronic inflammation, leading to the development of atrophic gastritis, intestinal metaplasia, and eventually gastric cancer. H. pylori infection is responsible for approximately 75% of all gastric cancer cases worldwide. However, not all individuals infected with H. pylori develop gastric cancer, suggesting that additional factors, such as host genetics and environmental factors, may influence the development of the disease.
C. Diet and lifestyle factors:
Certain dietary and lifestyle factors have been linked to an increased risk of gastric cancer. These include diets high in salt, smoked or processed meats, and low in fruits and vegetables. Consumption of foods contaminated with nitrites and nitrates, which can be converted to carcinogenic nitrosamines in the stomach, may also increase the risk. Other lifestyle factors that may contribute to gastric cancer include tobacco smoking, heavy alcohol consumption, and obesity.
D. Environmental factors:
Environmental factors, such as exposure to certain chemicals or substances, have been implicated in the development of gastric cancer. For example, exposure to asbestos, ionizing radiation, and certain occupational hazards, such as working in the rubber industry, have been associated with an increased risk of gastric cancer. However, these factors contribute to a small proportion of gastric cancer cases compared to other risk factors, such as H. pylori infection and genetic predisposition.
E. Age and gender:
The risk of developing gastric cancer increases with age, with most cases occurring in individuals over the age of 50. Gastric cancer is also more common in men than in women, with a male-to-female ratio of approximately 2:1.
F. Chronic gastritis and other medical conditions:
Chronic inflammation of the stomach lining, known as gastritis, can increase the risk of developing gastric cancer. In addition to H. pylori infection, other causes of gastritis include autoimmune gastritis and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). Patients with pernicious anemia, a condition that results in vitamin B12 deficiency due to the inability to absorb the vitamin, are also at an increased risk of gastric cancer. Other medical conditions that have been associated with a higher risk of gastric cancer include gastric polyps and a history of partial gastrectomy.

III. Symptoms and Diagnosis
A. Common symptoms:
In the early stages, gastric cancer often does not cause any symptoms or may present with nonspecific symptoms that can be mistaken for other gastrointestinal conditions. As the cancer progresses, patients may experience a range of symptoms, including:
1. Abdominal pain or discomfort, typically in the upper abdomen
2. Indigestion or heartburn
3. Loss of appetite
4. Unintended weight loss
5. Nausea and vomiting, sometimes with blood
6. Difficulty swallowing or a sensation of food getting stuck
7. Feeling full quickly after eating, even small amounts of food
8. Fatigue or weakness
9. Anemia (low red blood cell count), often due to bleeding from the tumor
10. Swelling or fluid buildup in the abdomen (ascites)
It is essential to consult a healthcare professional if any of these symptoms persist, as early diagnosis and treatment can significantly improve the prognosis for gastric cancer.
B. Diagnostic tools and techniques:
1. Endoscopy:
Endoscopy is a key diagnostic tool for gastric cancer. A flexible tube with a light and camera at its tip, called an endoscope, is inserted through the mouth and down the esophagus to examine the stomach lining. The procedure allows the doctor to visualize any abnormalities and obtain tissue samples for further analysis.
2. Biopsy:
A biopsy involves taking a small sample of tissue from the suspicious area in the stomach for examination under a microscope. This is typically done during the endoscopy procedure. A pathologist analyzes the tissue sample to determine whether cancer cells are present and, if so, the type of cancer and its grade.
3. Imaging techniques (CT scan, MRI, PET scan):
Imaging techniques such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans can provide detailed images of the stomach and surrounding structures. These imaging modalities help determine the extent of the cancer, its spread to nearby organs or lymph nodes, and the presence of metastases in distant parts of the body.
4. Blood tests:
Blood tests can provide information about the patient’s overall health and may detect the presence of certain substances, known as tumor markers, that can be associated with gastric cancer. The most common tumor marker for gastric cancer is carcinoembryonic antigen (CEA), although it is not specific to gastric cancer and can be elevated in other conditions as well.
C. Staging of gastric cancer:
Once gastric cancer has been diagnosed, it is essential to determine the stage of the disease, which indicates how advanced the cancer is and whether it has spread to other parts of the body. Staging is based on the tumor size (T), the involvement of nearby lymph nodes (N), and the presence of distant metastases (M). Staging plays a critical role in determining the most appropriate treatment plan and predicting the patient’s prognosis. The staging system commonly used for gastric cancer is the TNM system developed by the American Joint Committee on Cancer (AJCC).

IV. Treatment Approaches
A. Surgery:
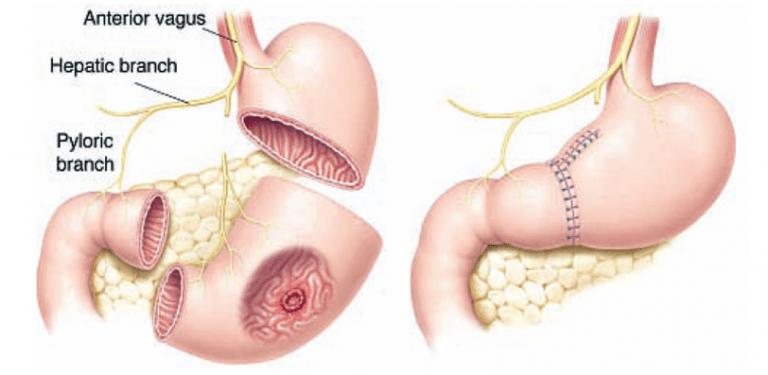
Surgery is often the primary treatment for gastric cancer, especially in the early stages of the disease. The type of surgery depends on the location, size, and stage of the tumor.
1. Types of surgery:
a. Subtotal gastrectomy: This procedure involves removing the part of the stomach affected by the tumor, along with nearby lymph nodes and sometimes parts of other organs if the cancer has spread. The remaining healthy part of the stomach is then connected to the small intestine.
b. Total gastrectomy: In this procedure, the entire stomach is removed along with nearby lymph nodes and sometimes parts of other organs if the cancer has spread. The esophagus is then directly connected to the small intestine.
c. Endoscopic resection: This minimally invasive procedure is suitable for very early-stage gastric cancers that have not spread beyond the inner lining of the stomach. The cancerous tissue is removed through an endoscope, without the need for open surgery.
2. Risks and benefits:
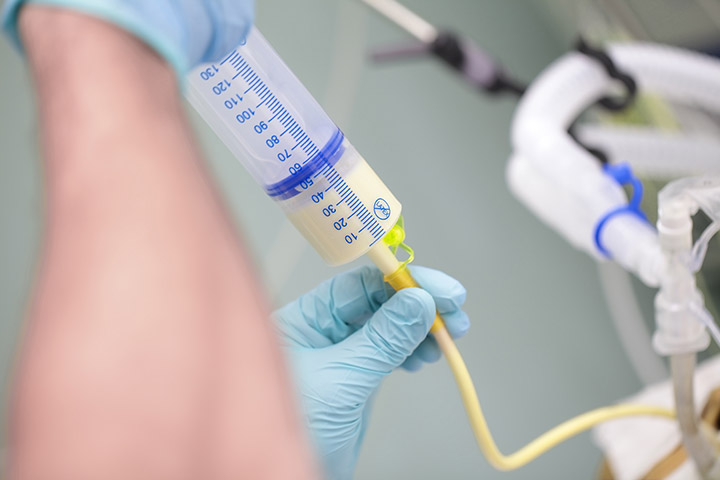
Surgery can be curative if the cancer is detected at an early stage and has not spread to other organs or tissues. However, surgery carries inherent risks, such as bleeding, infection, and complications related to anesthesia. Additionally, patients who have undergone gastrectomy may experience long-term side effects, such as difficulty eating, malabsorption of nutrients, and weight loss.
B. Chemotherapy:
Chemotherapy uses drugs to kill cancer cells or stop their growth. It can be used before surgery (neoadjuvant therapy) to shrink the tumor, making it easier to remove, or after surgery (adjuvant therapy) to eliminate any remaining cancer cells and reduce the risk of recurrence.
1. Neoadjuvant and adjuvant chemotherapy:
a. Neoadjuvant chemotherapy is administered before surgery to shrink the tumor and increase the likelihood of complete surgical removal. This approach may also make less invasive surgical techniques possible.
b. Adjuvant chemotherapy is given after surgery to kill any remaining cancer cells, reducing the risk of the cancer coming back. The decision to use adjuvant chemotherapy depends on the stage of the cancer and the risk of recurrence.
2. Side effects and management:
Chemotherapy can cause various side effects, such as nausea, vomiting, hair loss, fatigue, and increased risk of infection. Most side effects are temporary and can be managed with medications and supportive care. The specific side effects experienced depend on the type and dosage of chemotherapy drugs used.
C. Radiation therapy:
Radiation therapy uses high-energy rays or particles to destroy cancer cells. It can be used before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
1. External beam radiation therapy:
This is the most common type of radiation therapy for gastric cancer. A machine outside the body directs high-energy beams at the tumor site. Treatment is typically given in daily sessions over several weeks.
2. Brachytherapy:
In brachytherapy, radioactive seeds or pellets are placed directly into or near the tumor. This approach allows for a higher radiation dose to be delivered directly to the cancer cells, minimizing damage to surrounding healthy tissue. Brachytherapy is less commonly used for gastric cancer but may be considered in specific situations.
3. Side effects and management:
Radiation therapy can cause side effects such as skin irritation, fatigue, nausea, vomiting, and diarrhea. Most side effects are temporary and can be managed with medications and supportive care. Long-term side effects may include damage to nearby organs and tissues.
D. Targeted therapy and immunotherapy:
These newer treatment options aim to target specific characteristics of cancer cells or enhance the body’s immune response against cancer cells.
1. Monoclonal antibodies:
Monoclonal antibodies are laboratory made proteins that can target specific proteins on cancer cells or in the surrounding environment, interfering with cancer cell growth and survival. Trastuzumab (Herceptin) is a monoclonal antibody used to treat HER2-positive gastric cancer, a subtype of the disease with an overexpression of the HER2 protein.
2. Immune checkpoint inhibitors:
Immune checkpoint inhibitors are a type of immunotherapy that helps the immune system recognize and attack cancer cells. These drugs block proteins that act as “brakes” on immune cells, allowing the immune system to more effectively target and destroy cancer cells. Examples of immune checkpoint inhibitors used in the treatment of gastric cancer include pembrolizumab (Keytruda) and nivolumab (Opdivo), which target the PD-1 protein.
3. Emerging therapies and clinical trials:
New targeted therapies and immunotherapies are continuously being developed and tested in clinical trials. These trials aim to identify more effective and less toxic treatment options for gastric cancer. Patients with advanced or recurrent gastric cancer who have exhausted standard treatment options may consider enrolling in a clinical trial.
E. Palliative care and symptom management:
Palliative care is an essential aspect of gastric cancer treatment, particularly for patients with advanced or metastatic disease. The goal of palliative care is to improve the patient’s quality of life by managing symptoms, such as pain, nausea, and difficulty eating, and addressing emotional, spiritual, and practical concerns. Palliative care can be provided alongside other cancer treatments and should be tailored to the individual patient’s needs and preferences.
V. Prevention and Early Detection
A. Primary prevention strategies:
Primary prevention aims to reduce the risk of developing gastric cancer by addressing modifiable risk factors and promoting a healthy lifestyle.
1. H. pylori eradication:
Screening for and treating H. pylori infection can help prevent gastric cancer, as the bacterium is responsible for the majority of cases. Antibiotics can effectively eradicate H. pylori infection and reduce the risk of developing gastric cancer, especially if treated at an early stage of the infection.
2. Dietary modifications:
Adopting a healthy diet can lower the risk of gastric cancer. This includes consuming a diet rich in fruits and vegetables, whole grains, and lean proteins while limiting the intake of salt, processed meats, and smoked or pickled foods. Consuming foods high in antioxidants and other cancer-fighting nutrients can also help protect against gastric cancer.
3. Tobacco and alcohol control:
Smoking cessation and limiting alcohol consumption can reduce the risk of developing gastric cancer. Public health policies and interventions aimed at reducing tobacco and alcohol use can play a crucial role in preventing gastric cancer at the population level.
4. Maintaining a healthy weight:
Obesity is a risk factor for gastric cancer, and maintaining a healthy weight through a balanced diet and regular physical activity can help reduce the risk.
B. Early detection and screening:
Early detection of gastric cancer can significantly improve the chances of successful treatment and long-term survival. However, routine screening for gastric cancer is not currently recommended for the general population in most countries, as the benefits do not outweigh the risks and costs for individuals at average risk.
1. High-risk populations:
Screening may be considered for individuals at high risk of gastric cancer, such as those with a strong family history of the disease, hereditary gastric cancer syndromes, or known H. pylori infection. In some countries with high gastric cancer incidence, such as Japan and South Korea, mass screening programs have been implemented using upper gastrointestinal endoscopy and/or barium swallow tests.
2. Awareness and education:
Increasing public awareness of gastric cancer, its risk factors, and symptoms can help promote early detection and timely intervention. Healthcare providers should educate their patients about the warning signs of gastric cancer and encourage them to seek medical attention if they experience persistent or concerning symptoms.
3. Advances in diagnostic techniques:
Emerging diagnostic techniques, such as minimally invasive endoscopic methods, blood tests for tumor markers, and molecular biomarkers, may improve the early detection of gastric cancer in the future. Ongoing research and development in this area could help identify more sensitive and specific diagnostic tools that can be used for screening and early detection in high-risk populations.