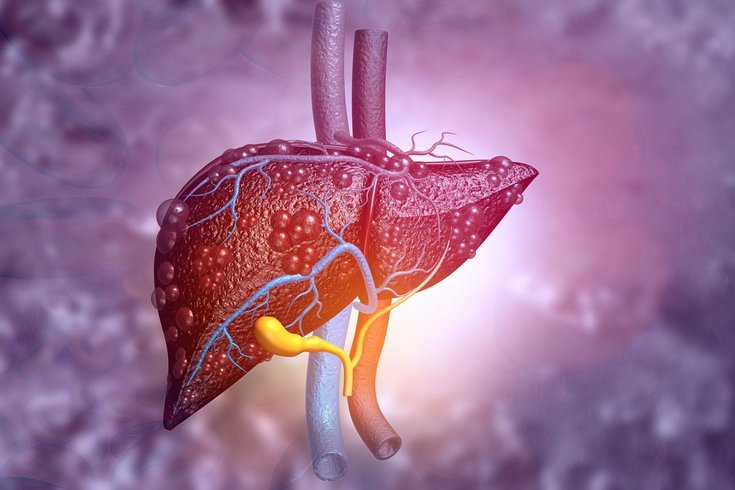
Viral hepatitis symptoms and treatment
Viral hepatitis, a group of infectious diseases primarily affecting the liver, has emerged as a significant global health concern. With various strains of the virus causing distinct forms of the disease, understanding the symptoms and available treatment options is crucial for effective management and prevention.
Symptoms of Viral Hepatitis: Viral hepatitis encompasses several types, including Hepatitis A, B, C, D, and E. While each strain exhibits unique characteristics, there are common symptoms that may manifest across different types:
- Fatigue: Persistent and unexplained fatigue is a prevalent symptom of viral hepatitis, often accompanied by a general feeling of weakness.
- Jaundice: Yellowing of the skin and eyes, known as jaundice, is a hallmark sign of liver dysfunction in hepatitis. It occurs due to the buildup of bilirubin, a yellow pigment, in the body.
- Abdominal Discomfort: Many individuals with viral hepatitis experience abdominal pain, tenderness, or discomfort, often in the area of the liver.
- Nausea and Vomiting: Hepatitis can lead to nausea, vomiting, and a reduced appetite, contributing to weight loss and malnutrition.
- Dark Urine and Pale Stools: Changes in urine color (darkening) and stool color (paling) can indicate hepatitis-related liver dysfunction.
- Joint Pain: Some types of viral hepatitis, such as Hepatitis B, may cause joint pain and muscle aches.
- Fever: Fever is a common response to infection, and it can accompany viral hepatitis, particularly during the acute phase.
- Flu-Like Symptoms: Early stages of viral hepatitis can mimic flu-like symptoms, including fever, headache, and muscle soreness.
Treatment Approaches: Effective management of viral hepatitis involves a combination of medical interventions and lifestyle modifications, depending on the specific type of hepatitis:
- Hepatitis A: There is no specific antiviral treatment for Hepatitis A. Supportive care, including rest, hydration, and a balanced diet, is crucial for recovery. Vaccination is the primary preventive measure.
- Hepatitis B: Chronic Hepatitis B may require antiviral medications to reduce viral load and slow disease progression. Vaccination is recommended for prevention.
- Hepatitis C: Antiviral medications have revolutionized the treatment of Hepatitis C, with newer direct-acting antiviral drugs offering high cure rates and fewer side effects.
- Hepatitis D: Hepatitis D is unique as it can only occur in individuals already infected with Hepatitis B. Preventing Hepatitis B through vaccination is key to avoiding Hepatitis D. Antiviral therapy may also be used.
- Hepatitis E: In most cases, Hepatitis E is self-limiting and resolves on its own. Supportive care is recommended, particularly for pregnant women who are at a higher risk of severe complications.
Preventive Measures: Viral hepatitis can be prevented through various strategies:
- Vaccination: Vaccines are available for Hepatitis A and B. Immunization plays a crucial role in reducing the incidence of these infections.
- Safe Hygiene Practices: Practicing good hygiene, such as washing hands thoroughly, avoiding contaminated water and food, and practicing safe sex, can help prevent the spread of hepatitis.
- Needle Safety: Avoid sharing needles or other drug paraphernalia to prevent the transmission of Hepatitis B and C.
- Screening and Testing: Regular screening and testing for Hepatitis B and C can help identify infections early, allowing for timely intervention.
- Mother-to-Child Transmission Prevention: Pregnant women with Hepatitis B should receive appropriate medical care to prevent transmission of the virus to their infants.
Emerging Research and Future Outlook: In recent years, significant strides have been made in the field of viral hepatitis research, leading to a better understanding of the viruses, their modes of transmission, and innovative treatment approaches. As we delve deeper into this intricate realm, promising developments are on the horizon:
- Improved Diagnostics: Researchers are working on more accurate and accessible diagnostic tools to detect viral hepatitis at an earlier stage. These advancements can lead to timely interventions, reducing the risk of severe liver damage.
- Novel Treatment Strategies: Beyond antiviral medications, scientists are exploring novel treatment strategies such as immune-modulating therapies and combination therapies. These approaches aim to enhance the body’s natural defense mechanisms against the virus.
- Global Awareness and Advocacy: Efforts to raise awareness about viral hepatitis are gaining momentum. International organizations, governments, and healthcare providers are collaborating to educate communities about prevention, transmission, and available resources.
- Elimination Goals: Many countries have set ambitious goals to eliminate viral hepatitis as a public health threat. These goals encompass increased vaccination coverage, enhanced screening programs, and improved access to treatment for affected individuals.
- Targeting High-Risk Populations: Tailored interventions are being developed to address specific high-risk populations, such as injecting drug users and individuals with compromised immune systems. These efforts aim to break the cycle of transmission and reduce new infections.
- Combating Stigma: Stigmatization of individuals with viral hepatitis remains a challenge. Advocacy campaigns are working to dispel myths, reduce discrimination, and encourage open dialogue to create a more supportive environment for those affected.
- Integration of Services: Healthcare systems are evolving to integrate viral hepatitis services with other healthcare programs. This approach facilitates early detection and comprehensive care, contributing to better patient outcomes.
- Research into Hepatitis E: As the understanding of Hepatitis E evolves, research is focusing on improving the management of this virus, especially in pregnant women and immunocompromised individuals.
In the quest to address viral hepatitis comprehensively, collaboration among healthcare professionals, researchers, policymakers, and communities is paramount. By embracing these multifaceted strategies, we move closer to a world where viral hepatitis is no longer a widespread threat, and individuals can lead healthier lives free from the burden of this disease.
In summary, the landscape of viral hepatitis is rapidly evolving, driven by advancements in research, innovative treatments, and a global commitment to prevention. As we navigate this ever-changing terrain, a holistic approach encompassing early diagnosis, effective treatment, and community engagement holds the key to minimizing the impact of viral hepatitis and paving the way for a healthier future.