Signs of a woman having a heart attack or stroke
Stroke and heart attack are two of the most common medical emergencies that can happen to anyone, regardless of age or gender. Although both conditions are caused by a disruption of blood flow to vital organs, they have distinct differences in their symptoms and causes. It is crucial to know the difference between stroke and heart attack symptoms to seek immediate medical attention and receive appropriate treatment. This article aims to explore the differences between stroke and heart attack symptoms, risk factors, and treatment options. By raising awareness about these conditions, we can better protect ourselves and our loved ones from the devastating effects of stroke and heart attack.
1. Overview of Stroke and Heart Attack
1.1. Definition and types of stroke
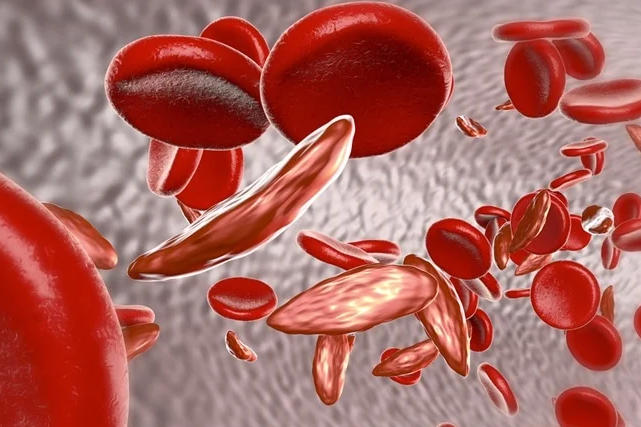
A stroke, also known as a cerebrovascular accident (CVA), is a medical emergency that occurs when the blood flow to a part of the brain is interrupted or reduced. This deprives the brain tissue of oxygen and nutrients, leading to the death of brain cells within minutes. There are two main types of stroke:
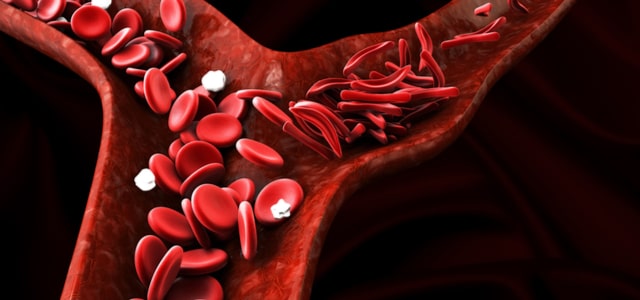
a. Ischemic stroke: This is the most common type of stroke, accounting for about 87% of all cases. It occurs when a blood clot blocks or narrows the blood vessels that supply the brain. Ischemic strokes can be further divided into two categories: thrombotic stroke, where a clot forms in the arteries directly supplying the brain, and embolic stroke, where a clot forms elsewhere in the body and travels to the brain.
b. Hemorrhagic stroke: This type of stroke is less common but more severe. It occurs when a blood vessel in the brain ruptures, causing bleeding into the surrounding brain tissue. Hemorrhagic strokes can be further divided into two categories: intracerebral hemorrhage, where bleeding occurs within the brain tissue, and subarachnoid hemorrhage, where bleeding occurs between the brain and the surrounding membrane.
1.2. Definition and types of heart attack
A heart attack, also known as a myocardial infarction (MI), is a medical emergency that occurs when the blood flow to a part of the heart is blocked, usually by a blood clot. This interruption in blood flow can damage or destroy part of the heart muscle. There are two main types of heart attacks based on the extent of the artery blockage:
a. ST-segment elevation myocardial infarction (STEMI): This type of heart attack is characterized by a complete blockage of the coronary artery, resulting in extensive damage to the heart muscle. STEMI is considered more severe and requires immediate treatment to restore blood flow and minimize damage.
b. Non-ST-segment elevation myocardial infarction (NSTEMI): This type of heart attack involves a partial blockage of the coronary artery, resulting in a smaller area of damage to the heart muscle. NSTEMI is less severe than STEMI but still requires prompt medical attention and treatment.
1.3. Prevalence and impact on public health
Strokes and heart attacks are both major causes of death and disability worldwide. According to the World Health Organization (WHO), strokes are the second leading cause of death globally, accounting for approximately 11% of total deaths. Heart attacks, on the other hand, are the leading cause of death in many countries.
Both conditions also contribute significantly to the global burden of disease, with survivors often experiencing long-term disabilities and reduced quality of life. Stroke and heart attack prevention, early detection, and treatment are crucial components of public health strategies to reduce the impact of these conditions on individuals, families, and healthcare systems.
2. Pathophysiology and Risk Factors
2.1. Pathophysiology of stroke
The pathophysiology of stroke involves the interruption of blood flow to a part of the brain, leading to the death of brain cells and the subsequent loss of function in the affected areas. In ischemic strokes, this interruption occurs due to a blood clot blocking or narrowing the blood vessels that supply the brain. The clot can form within the brain’s blood vessels (thrombotic stroke) or elsewhere in the body and travel to the brain (embolic stroke).
In hemorrhagic strokes, the interruption of blood flow occurs due to the rupture of a blood vessel in the brain. This can lead to bleeding within the brain tissue itself (intracerebral hemorrhage) or between the brain and the surrounding membrane (subarachnoid hemorrhage). In both cases, the bleeding causes an increase in pressure within the skull, which can damage or compress surrounding brain tissue and impair brain function.
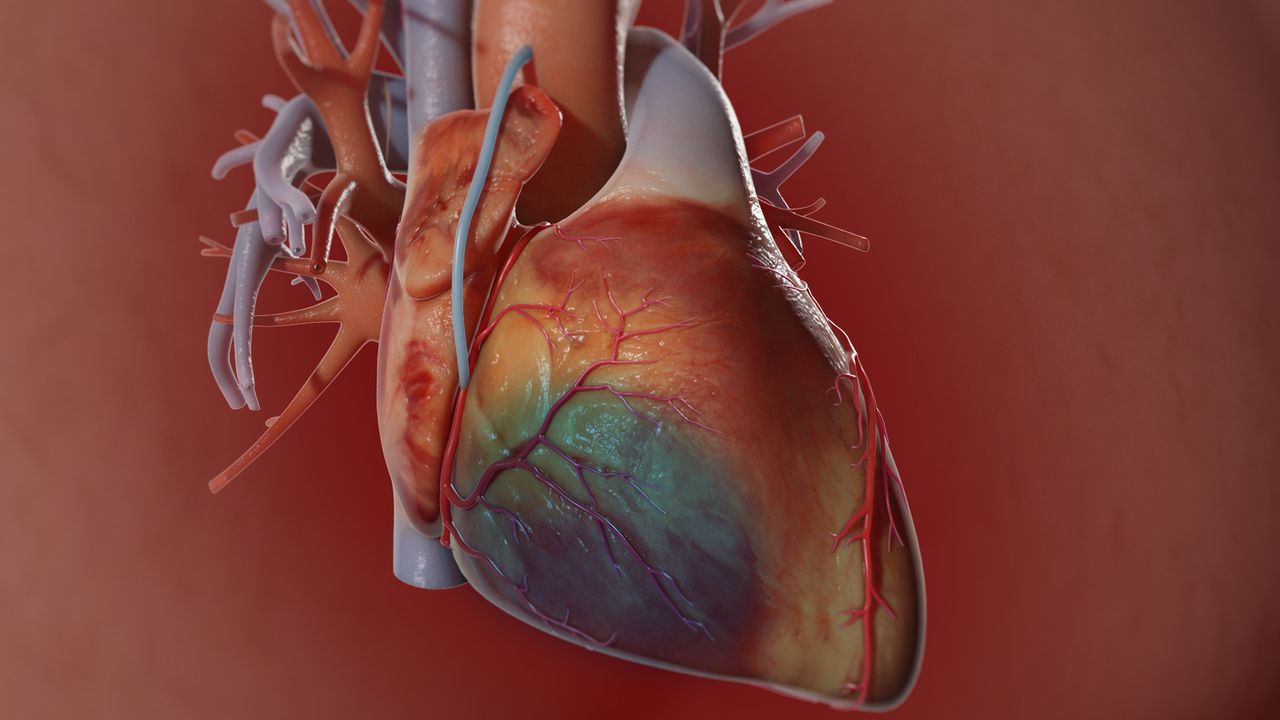
2.2. Pathophysiology of heart attack
The pathophysiology of a heart attack involves the interruption of blood flow to a part of the heart muscle, typically due to the formation of a blood clot. The clot usually forms in a coronary artery that has been narrowed or blocked by atherosclerosis, a condition characterized by the buildup of fatty deposits (plaque) inside the artery walls. When blood flow is restricted, the heart muscle becomes deprived of oxygen and nutrients, leading to damage or death of the affected tissue.
In STEMI heart attacks, the coronary artery is completely blocked, causing extensive damage to the heart muscle. In NSTEMI heart attacks, the blockage is partial, resulting in less extensive damage. In both cases, the interruption of blood flow can lead to the development of abnormal heart rhythms (arrhythmias) and potentially heart failure if left untreated.
2.3. Common risk factors for stroke and heart attack
Several risk factors contribute to the development of both stroke and heart attack. Some of the most common shared risk factors include:
a. Age: The risk of both conditions increases with age, particularly after the age of 55.
b. Hypertension: High blood pressure is a significant risk factor for both stroke and heart attack, as it can damage blood vessels and contribute to atherosclerosis.
c. Diabetes: Diabetes increases the risk of both conditions by damaging blood vessels and increasing the likelihood of blood clot formation.
d. High cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to the buildup of plaque in the arteries, increasing the risk of both stroke and heart attack.
e. Smoking: Smoking damages blood vessels and increases the risk of atherosclerosis, blood clots, and inflammation, contributing to the risk of both stroke and heart attack.
f. Obesity: Excess body weight is associated with an increased risk of both stroke and heart attack, as it can contribute to hypertension, diabetes, and high cholesterol levels.
g. Family history: A family history of stroke or heart attack can indicate a genetic predisposition to these conditions.
2.4. Unique risk factors for stroke
In addition to the shared risk factors, some risk factors are more specific to stroke, including:
a. Atrial fibrillation: An irregular heart rhythm that increases the risk of blood clot formation in the heart, which can then travel to the brain and cause an embolic stroke.
b. Previous stroke or transient ischemic attack (TIA): Having a history of stroke or TIA increases the risk of a subsequent stroke.
c. Race: Some racial and ethnic groups, such as African Americans, have a higher risk of stroke than others due to genetic factors and a higher prevalence of hypertension and diabetes.

3. Signs and Symptoms of Stroke
Stroke symptoms typically occur suddenly and can vary depending on the part of the brain that is affected. The most common signs and symptoms of a stroke include:
3.1. Sudden onset of neurological deficits
A stroke can cause sudden weakness, numbness, or paralysis on one side of the body, usually affecting the face, arm, or leg. This is due to the interruption of blood flow to the part of the brain that controls muscle function.
3.2. Facial drooping, arm weakness, and speech difficulties
One of the most recognizable signs of a stroke is facial drooping, which occurs when the muscles on one side of the face become weak or paralyzed. This can cause the mouth or eye to droop and may make it difficult to smile or close the eye. Additionally, arm weakness and speech difficulties, such as slurred or garbled speech, can be indicative of a stroke.
3.3. Vision problems
A stroke can cause sudden vision disturbances, such as blurred or double vision, or even temporary or permanent loss of vision in one or both eyes. This occurs when the part of the brain responsible for vision is affected by the stroke.
3.4. Balance and coordination issues
A stroke can affect a person’s balance and coordination, leading to difficulty walking, dizziness, or loss of balance. This can be caused by damage to the parts of the brain that control movement and balance.
3.5. Severe headache with no known cause
A sudden, severe headache with no apparent cause can be a sign of a stroke, particularly in the case of a hemorrhagic stroke. The headache may be accompanied by other stroke symptoms or may occur on its own. It is important to seek immediate medical attention if experiencing a sudden, severe headache, especially if it is unlike any previous headaches or if it is accompanied by other stroke symptoms.
It is crucial to recognize the signs of a stroke and seek immediate medical attention, as prompt treatment can significantly improve outcomes and reduce the risk of long-term disability. The acronym FAST (Face, Arm, Speech, Time) can be a helpful tool for remembering the key signs of a stroke and the importance of seeking timely medical care.

4. Signs and Symptoms of Heart Attack
Heart attack symptoms can vary among individuals, and some people may experience mild or atypical symptoms. However, there are several common signs and symptoms that may indicate a heart attack:
4.1. Chest pain or discomfort
Chest pain is one of the most common symptoms of a heart attack. This pain may feel like a pressure, squeezing, fullness, or tightness in the center of the chest. The pain can be mild or severe and may come and go or persist. Although chest pain is often considered the hallmark symptom of a heart attack, not all heart attacks cause chest pain, and some people may experience discomfort in other areas.
4.2. Shortness of breath
Shortness of breath, or difficulty breathing, can occur during a heart attack even if there is no chest pain. This symptom may be the result of the heart’s inability to pump blood effectively, leading to decreased oxygen levels in the body. Shortness of breath may be accompanied by a feeling of lightheadedness or dizziness.
4.3. Pain in the arms, neck, jaw, back, or stomach
Pain or discomfort during a heart attack may not be limited to the chest. Some people may experience pain in one or both arms, the neck, jaw, back, or stomach. This type of pain, called referred pain, occurs when the nerves that serve the heart also serve other areas of the body, causing pain signals to be perceived in those areas rather than in the heart itself.
4.4. Cold sweats and lightheadedness
A heart attack can cause cold sweats, which may be accompanied by lightheadedness or dizziness. These symptoms may be the result of the body’s response to the stress of the heart attack and the reduced blood flow and oxygen levels.
4.5. Nausea and vomiting
Nausea and vomiting can also be symptoms of a heart attack, particularly in women. These symptoms may be caused by the activation of the body’s stress response and the release of stress hormones, as well as reduced blood flow to the digestive system.
It is important to recognize the signs and symptoms of a heart attack and seek immediate medical attention, as early treatment can significantly improve outcomes and reduce the risk of permanent damage to the heart muscle. Remember that heart attack symptoms can vary among individuals, and some people may experience mild or atypical symptoms. If you suspect a heart attack, it is better to err on the side of caution and seek medical help promptly.
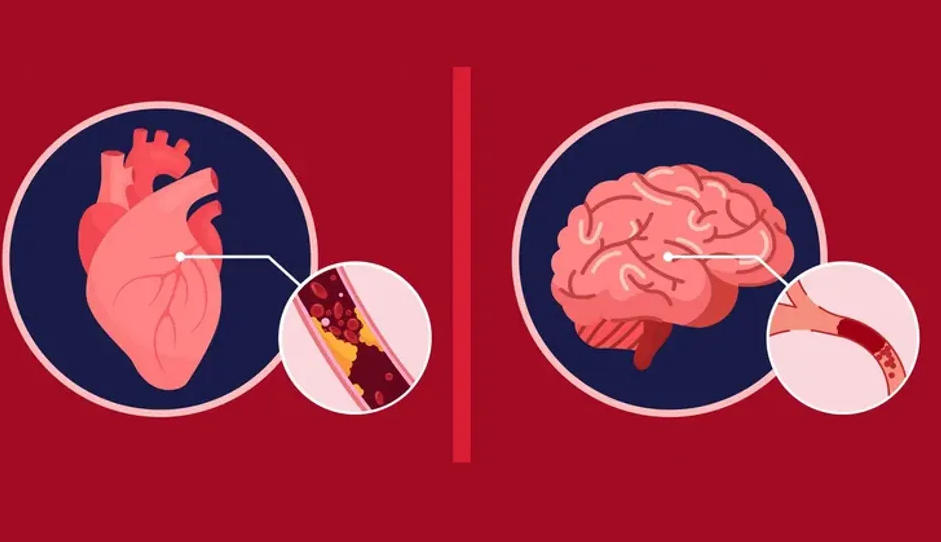
5. Comparison of Stroke and Heart Attack Symptoms
While both stroke and heart attack are medical emergencies caused by the interruption of blood flow to vital organs, their symptoms can differ due to the organs affected. Recognizing the differences between the symptoms of these conditions is crucial for seeking appropriate and timely medical care.
5.1. Similarities in symptoms
There are some overlapping symptoms between stroke and heart attack, which can sometimes cause confusion. These shared symptoms may include:
a. Sudden onset of symptoms: Both stroke and heart attack symptoms typically appear suddenly and without warning.
b. Weakness or numbness on one side of the body: While this is more common in stroke, some heart attack patients may also experience weakness or numbness in the arm or upper body.
c. Lightheadedness or dizziness: Both conditions can cause lightheadedness or dizziness due to reduced blood flow and oxygen levels in the body.
5.2. Differences in symptoms
Despite some similarities, there are key differences between the symptoms of stroke and heart attack:
a. Chest pain or discomfort: This is a hallmark symptom of a heart attack but is not typically associated with a stroke.
b. Facial drooping, arm weakness, and speech difficulties: These are classic stroke symptoms and are not typically seen in heart attack patients.
c. Vision problems: Sudden vision disturbances are more indicative of a stroke than a heart attack.
d. Balance and coordination issues: These symptoms are more common in stroke patients, as the affected brain areas control movement and balance.
e. Pain in other areas of the body: Heart attack patients may experience pain in the arms, neck, jaw, back, or stomach, while stroke patients usually do not have pain in these areas.
f. Nausea and vomiting: These symptoms are more common in heart attack patients, especially women, but are not typical symptoms of a stroke.
5.3. Importance of recognizing the differences
Recognizing the differences between stroke and heart attack symptoms is essential for several reasons:
a. Seeking appropriate medical care: Knowing the symptoms of each condition can help individuals identify the need for medical attention and seek the appropriate care.
b. Faster diagnosis and treatment: Being able to distinguish between stroke and heart attack symptoms can help healthcare professionals quickly diagnose and initiate the proper treatment, which can improve outcomes and reduce the risk of long-term disability.
c. Prompt intervention: Both stroke and heart attack require immediate intervention to restore blood flow to the affected organ and minimize damage. Recognizing the differences in symptoms can help ensure that patients receive the most effective treatment as quickly as possible.

6. Treatment and Management of Stroke and Heart Attack
The treatment and management of stroke and heart attack aim to restore blood flow, minimize damage to the affected organ, and prevent complications. The specific treatment approach depends on the type and severity of the condition, as well as the patient’s overall health.
6.1. Treatment of stroke
The treatment of stroke depends on whether it is an ischemic or hemorrhagic stroke:
a. Ischemic stroke: The primary treatment goal is to restore blood flow to the brain as quickly as possible. This can be achieved using clot-busting medications, such as tissue plasminogen activator (tPA), which can dissolve the clot and improve blood flow. Another treatment option is mechanical thrombectomy, a procedure in which a catheter is inserted into the blocked blood vessel to remove the clot directly. Time is crucial for ischemic stroke treatment, and early intervention can significantly improve outcomes.
b. Hemorrhagic stroke: The treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in the brain. This may involve medications to lower blood pressure, reduce brain swelling, and prevent seizures. In some cases, surgery may be necessary to repair the damaged blood vessel or relieve pressure within the skull.
6.2. Treatment of heart attack
The treatment of a heart attack aims to restore blood flow to the heart muscle and minimize damage. Treatment options include:
a. Medications: Various medications can be used to break down clots, prevent new clot formation, reduce pain, and relax blood vessels. These may include aspirin, antiplatelet drugs, anticoagulants, pain relievers, and nitroglycerin.
b. Percutaneous coronary intervention (PCI): Also known as angioplasty, PCI is a procedure in which a catheter is inserted into the blocked coronary artery to widen the artery and restore blood flow. A stent may be placed to keep the artery open.
c. Coronary artery bypass grafting (CABG): In some cases, a surgical procedure called CABG may be performed to bypass the blocked artery and create a new route for blood flow to the heart muscle.
6.3. Rehabilitation and secondary prevention
Following a stroke or heart attack, rehabilitation plays a crucial role in helping patients regain lost function and improve their quality of life. Rehabilitation may include physical therapy, occupational therapy, and speech therapy, depending on the specific needs of the patient.
Secondary prevention strategies are also essential for reducing the risk of future events. These may involve lifestyle modifications (e.g., adopting a healthy diet, increasing physical activity, quitting smoking), medications to manage risk factors (e.g., blood pressure, cholesterol, diabetes), and regular follow-up appointments with healthcare providers.
6.4. Importance of timely intervention
Time is a critical factor in the treatment and management of both stroke and heart attack. Early recognition of symptoms and prompt intervention can significantly improve outcomes, reduce the risk of long-term disability, and save lives. It is essential for individuals and healthcare professionals to be aware of the signs and symptoms of these conditions and to take appropriate action when they are suspected.