Is donating blood completely safe?
This article provides an extensive overview of blood donation, discussing its significance, the process, benefits, and potential drawbacks. The aim of this article is to educate readers on the importance of blood donation and address common concerns, in order to encourage informed decisions regarding this vital practice.

1. Introduction
1.1. Background and Significance
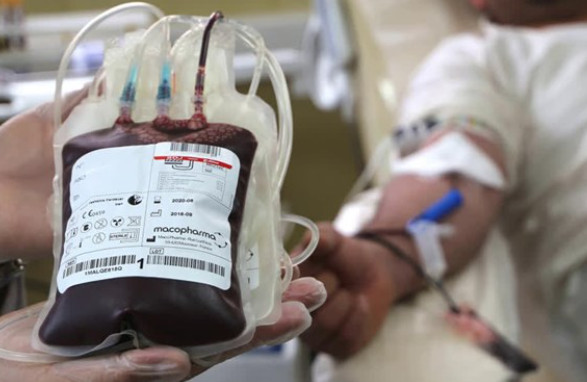
Blood donation is a critical practice in modern healthcare, as it allows for the collection, testing, and distribution of blood components to patients in need. Blood transfusions are required for a variety of medical conditions and emergencies, such as surgery, trauma, cancer treatments, and chronic illnesses. The demand for blood is constant, making regular donations essential to maintaining an adequate supply in blood banks and hospitals.
Blood donations not only save lives but also contribute to the overall improvement of public health. According to the World Health Organization (WHO), around 118.4 million blood donations are collected globally every year, with voluntary, unpaid blood donations being the cornerstone of a safe and sustainable blood supply. The selfless act of donating blood has a profound impact on the lives of recipients and their families.
1.2. Purpose and Scope
The purpose of this article is to provide a comprehensive understanding of blood donation, including its definition, the process, the benefits, and potential drawbacks. This article aims to educate readers about the importance of blood donation and address any concerns, misconceptions, or myths that may discourage potential donors from participating in this vital practice.
2. What is Blood Donation?
2.1. Definition and Overview
Blood donation is the voluntary act of giving blood, which is then processed and separated into its various components, such as red blood cells, plasma, and platelets, to be used for transfusions and medical treatments. Blood transfusions can be life-saving in various situations, including surgeries, accidents, cancer treatments, and chronic blood disorders. As blood has a limited shelf-life, and certain blood components have even shorter viability, there is a continuous need for new donations to replenish the blood supply.
2.2. Types of Blood Donations
There are several types of blood donations, each with a specific purpose and benefit. The four main types of blood donations are:
2.2.1. Whole Blood Donation
Whole blood donation is the most common and widely known type of blood donation. It involves the collection of blood as it is, without separating any of its components during the donation process. After collection, whole blood is typically separated into red blood cells, plasma, and platelets, which can be used for various medical treatments. The entire process takes approximately 45 minutes to an hour, and donors can give whole blood every 56 days.
2.2.2. Plasma Donation
Plasma donation, also known as plasmapheresis, involves the collection of plasma, the liquid component of blood that carries cells and proteins throughout the body. Plasma is crucial for clotting and supporting immunity. During plasma donation, blood is drawn from the donor, the plasma is separated from the other components, and the remaining blood elements are returned to the donor. This process takes around 1.5 to 2 hours, and donors can give plasma as frequently as every 28 days.
2.2.3. Platelet Donation
Platelet donation, or plateletpheresis, is the collection of platelets, the blood components responsible for clotting and preventing excessive bleeding. Platelet donation is particularly important for cancer patients, as treatments like chemotherapy can reduce their platelet count. Similar to plasma donation, the blood is drawn, platelets are separated, and the remaining blood components are returned to the donor. The process takes approximately 2 to 3 hours, and donors can give platelets every 7 days, up to 24 times per year.
2.2.4. Double Red Cell Donation
Double red cell donation, also known as apheresis, is the process of collecting twice the amount of red blood cells typically collected during a whole blood donation while returning the plasma and platelets to the donor. Red blood cells are vital for carrying oxygen throughout the body, making this type of donation especially helpful for patients with severe anemia or blood loss. Double red cell donation takes about 1.5 hours, and donors can give every 112 days.
Each type of blood donation serves a specific purpose and caters to different medical needs. By understanding these different types of donations, individuals can choose the most suitable option for them and contribute to the vital blood supply needed in the healthcare system.

3. The Blood Donation Process
3.1. Eligibility Criteria
Before donating blood, individuals must meet specific eligibility criteria to ensure the safety of both the donor and the recipient. Criteria may vary by country and blood center, but general requirements include:
– Age: Typically, donors must be between 17 and 65 years old, although some centers may accept donors as young as 16 with parental consent or as old as 70 if they have previously donated.
– Weight: Donors must usually weigh at least 110 pounds (50 kg).
– Health: Donors should be in good general health and feeling well on the day of donation. Some medical conditions or medications may temporarily or permanently disqualify individuals from donating.
– Travel history: Donors who have recently visited certain countries or regions may be deferred due to potential exposure to infections, such as malaria or Zika virus.
– Risk behaviors: High-risk behaviors, such as intravenous drug use or engaging in unprotected sex with multiple partners, may disqualify individuals from donating to protect the blood supply from potential infections.
It is essential to consult your local blood center or healthcare professional to determine your specific eligibility to donate blood.
3.2. The Donation Process Step-by-Step
The blood donation process typically consists of the following steps:
1. Registration: Upon arrival at the donation center or blood drive, donors provide their identification and complete a registration form with personal and contact information.
2. Medical history and mini-physical: Donors undergo a brief health assessment, which includes a questionnaire about their medical history, lifestyle, and travel history, as well as a mini-physical where blood pressure, pulse, temperature, and hemoglobin levels are checked.
3. Donation: If the donor is eligible, they proceed to the donation area where a trained staff member cleans the arm and inserts a sterile needle into the vein. The blood collection takes approximately 10 minutes for whole blood donation and longer for other types of donations.
4. Refreshments and recovery: After the donation, donors rest in a designated area, where they are provided with refreshments to help replenish their fluids and energy. Donors are encouraged to rest for at least 10-15 minutes before leaving the center.
3.3. Post-Donation Care and Recovery
After donating blood, it is essential to follow post-donation care guidelines to ensure a smooth recovery:
– Hydrate: Drink plenty of fluids to help replace the lost volume and prevent dizziness or fainting.
– Eat well: Consume a balanced meal within a few hours of donation, including iron-rich foods to replenish iron stores.
– Rest: Avoid strenuous activities and heavy lifting for at least 24 hours, as these may cause discomfort or dizziness.
– Monitor the donation site: Keep the bandage on for a few hours and avoid contact with water to minimize the risk of infection. If bleeding occurs, apply pressure and elevate the arm.
Donors typically recover within a day or two and can resume their normal activities. It is crucial to listen to your body and consult a healthcare professional if any concerns arise during recovery.

4. Benefits of Blood Donation
Blood donation offers numerous benefits, not only for the recipients but also for the donors and the healthcare system as a whole. Some of the primary advantages include:
4.1. Saving Lives and Improving Health
One of the most significant benefits of blood donation is its potential to save lives. Each donation can help up to three people, depending on how the blood is processed and used. Blood transfusions are essential for a variety of medical situations, including surgeries, accidents, cancer treatments, and chronic blood disorders. Donating blood directly contributes to the well-being and recovery of these patients, improving their quality of life.
4.2. Alleviating Blood Shortages
Regular blood donations are crucial in maintaining an adequate blood supply for hospitals and blood banks. Blood shortages can be detrimental, leading to the postponement of surgeries or the unavailability of blood for emergency situations. By donating blood, individuals help ensure that the healthcare system can respond effectively to the needs of patients requiring blood transfusions.
4.3. Benefits to the Donor
In addition to the positive impact on recipients, blood donation also offers several benefits to the donors:
4.3.1. Health Screenings
Before donating blood, donors undergo a mini-physical and a medical history review. This process provides an opportunity for a general health check-up, which may help identify any potential health concerns or risk factors. Additionally, donated blood is tested for various infectious diseases, such as HIV, hepatitis B and C, and syphilis. If any irregularities are detected, donors are informed and advised to consult a healthcare professional.
4.3.2. Psychological Well-being
Blood donation can contribute to a sense of satisfaction and fulfillment, as donors know that their actions directly benefit the lives of others. This altruistic act can lead to an increased sense of purpose and well-being, positively impacting the donor’s mental health.
4.3.3. Reduced Risk of Certain Health Conditions
Some studies have suggested that regular blood donation may be associated with a reduced risk of certain health conditions, such as heart disease and high blood pressure. This is thought to be due to the reduction of iron stores in the body, which can lower the risk of oxidation and inflammation. However, more research is needed to confirm these findings, and blood donation should not be considered a substitute for medical care or a healthy lifestyle.
5. Potential Drawbacks and Concerns of Blood Donation
While blood donation is a generally safe and beneficial practice, there are potential drawbacks and concerns that donors and healthcare providers should be aware of:
5.1. Physical Reactions and Risks
Some donors may experience mild to moderate physical reactions during or after blood donation, such as:
5.1.1. Fainting and Dizziness
Fainting, dizziness, or lightheadedness can occur during or after blood donation, especially in first-time donors or those who are more sensitive to blood loss. Proper hydration, a well-balanced meal before donating, and resting for a few minutes after the donation can help minimize these reactions.
5.1.2. Hematoma Formation
A hematoma is a collection of blood outside the blood vessels, which may occur if the needle punctures the vein or if pressure is not applied correctly after the donation. While usually harmless, hematomas can cause discomfort and may take several days to resolve.
5.1.3. Infection
Although rare, there is a small risk of infection at the needle insertion site due to improper sterilization or post-donation care. Following the post-donation guidelines provided by the blood center, such as keeping the bandage on and avoiding water contact, can help prevent infections.
5.2. Emotional and Psychological Reactions
Some donors may experience emotional or psychological reactions related to blood donation, such as anxiety or fear of needles. It is essential to communicate any concerns or discomfort with the healthcare staff, who can provide support and guidance during the donation process.
5.3. Misconceptions and Myths Surrounding Blood Donation
There are several misconceptions and myths surrounding blood donation that may discourage potential donors or create unnecessary concerns. Some common misconceptions include:
– Belief that blood donation is painful: While the needle insertion may cause mild discomfort, most donors report that the process is relatively painless.
– Concern about contracting diseases: Blood donation is a sterile procedure, and all needles and equipment are used only once before being discarded, ensuring that donors cannot contract diseases from donating blood.
– Fear of not having enough blood after donation: The human body has the capacity to regenerate the lost blood volume within 24 to 48 hours and fully replenish blood cells within a few weeks.
Educating potential donors about the facts and debunking misconceptions can help address these concerns and encourage more people to participate in blood donation.

6. The Future of Blood Donation
As the demand for blood and blood components continues to rise, there is a growing need for innovations and advancements in blood donation practices to ensure a sustainable and safe blood supply. Some of the key areas of focus include:
6.1. Technological Innovations
Emerging technologies have the potential to revolutionize blood donation by making the process more efficient, safer, and more accessible:
6.1.1. Automated Blood Collection Devices
These devices can increase the precision and efficiency of the blood collection process, reducing the risk of human error, and potentially increasing the yield of blood components from a single donation.
6.1.2. Improved Screening and Testing Methods
The development of more accurate and rapid screening and testing methods for bloodborne diseases can help enhance the safety of the blood supply and reduce the window period for detecting infections.
6.1.3. Mobile Apps and Digital Platforms
The use of mobile apps and digital platforms can streamline the donor recruitment process, facilitate appointment scheduling, and provide donors with relevant information and reminders, making blood donation more convenient and accessible.
6.2. Artificial Blood Alternatives
Research on artificial blood alternatives, such as oxygen-carrying molecules or lab-grown red blood cells, holds promise for reducing the reliance on human blood donations. While still in the early stages of development, these alternatives could potentially alleviate blood shortages and provide life-saving options for patients with rare blood types or those who require blood transfusions in emergency situations.
6.3. Expanding the Donor Base
Efforts to expand the donor base, such as raising awareness about the importance of blood donation, debunking myths and misconceptions, and developing targeted campaigns for underrepresented donor groups, can help increase the number of blood donations and ensure a more diverse blood supply.
6.4. Revisiting Donation Eligibility Criteria
Periodically reviewing and updating blood donation eligibility criteria based on the latest scientific evidence and public health data can help ensure the safety and sustainability of the blood supply while potentially expanding the pool of eligible donors.
In conclusion, the future of blood donation lies in embracing technological advancements, fostering innovative research, and promoting a culture of altruism and awareness around the importance of blood donation. By working together, donors, healthcare professionals, and researchers can contribute to a more efficient, safe, and sustainable blood donation system that meets the ever-growing demand for blood and blood components.