Comprehensive Analysis of Asthma: Causes, Diagnosis, and Treatment Strategies
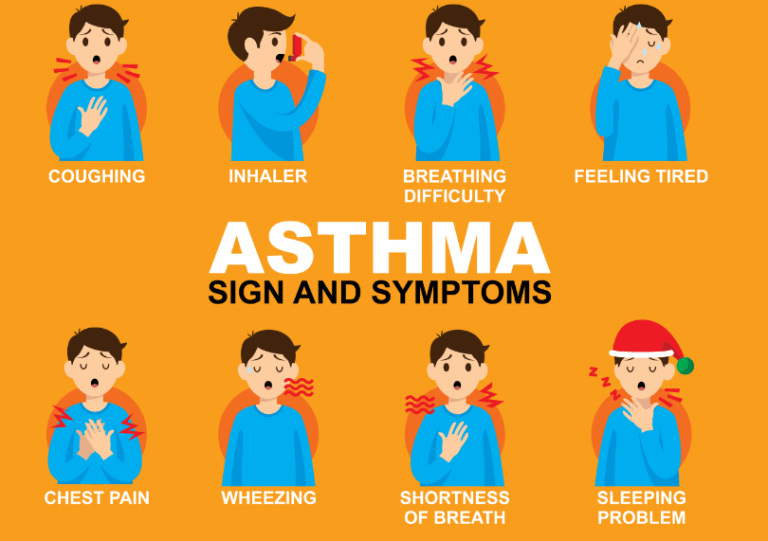
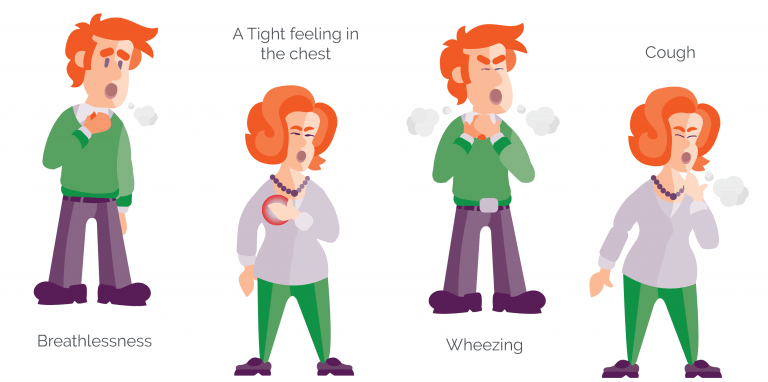
Asthma is a chronic respiratory disease that affects millions of people worldwide. It is a condition in which the airways in the lungs become narrow and inflamed, making it difficult to breathe. Asthma can cause symptoms such as coughing, wheezing, chest tightness, and shortness of breath, which can range from mild to severe.
The prevalence of asthma has been increasing over the past few decades, particularly in developed countries. It is estimated that approximately 300 million people worldwide have asthma, and this number is expected to continue to rise. Despite advances in treatment options, asthma remains a significant health concern, and it can have a significant impact on a person’s quality of life.
In this article, we will provide an overview of asthma, including its causes, symptoms, diagnosis, and treatment options. We will also discuss some of the challenges associated with managing asthma and provide tips for preventing asthma attacks. Finally, we will examine some of the ongoing research in the field of asthma and discuss potential future treatments for this chronic condition.
1. Introduction
1.1. Definition of Asthma
Asthma is a chronic inflammatory lung disease characterized by variable and recurring symptoms, airway obstruction, bronchial hyperresponsiveness, and underlying inflammation. It is a common condition affecting people of all ages, with symptoms ranging from mild to severe. Asthma is generally manifested through symptoms such as wheezing, shortness of breath, chest tightness, and coughing. The severity and frequency of these symptoms can vary among individuals and can be exacerbated by various triggers, such as allergens, irritants, and respiratory infections.
1.2. Epidemiology and Prevalence of Asthma
Asthma is a global public health concern affecting an estimated 339 million people worldwide, as of 2021. Its prevalence varies across different countries and regions, with higher rates observed in developed countries compared to developing countries. Asthma affects people of all ages; however, it often begins in childhood. According to the World Health Organization, asthma is the most common chronic disease among children.
The prevalence of asthma has been increasing over the past few decades, possibly due to a combination of factors, including increased urbanization, changes in lifestyle, and environmental exposure to allergens and pollutants. Asthma is responsible for a significant burden on healthcare systems, with considerable direct and indirect costs associated with the management of the disease and its impact on quality of life. Additionally, asthma accounts for a large number of hospitalizations, emergency department visits, and missed work and school days.
Despite the global impact of asthma, it remains underdiagnosed and undertreated in many regions. This underscores the importance of increasing awareness, improving diagnostic methods, and providing access to effective treatments for those affected by this chronic condition.
2. Pathophysiology of Asthma
2.1. Inflammation and Airway Hyperresponsiveness
The primary characteristic of asthma is chronic inflammation of the airways, which leads to airway hyperresponsiveness (AHR) and airflow obstruction. Inflammatory cells, such as eosinophils, mast cells, and T lymphocytes, play a crucial role in this process. These cells release various chemical mediators, such as histamine, leukotrienes, and cytokines, which cause bronchoconstriction, mucus production, and vascular leakage. This results in the narrowing of the airways and makes it difficult for air to pass through, leading to the characteristic symptoms of asthma.
Airway hyperresponsiveness is the increased sensitivity of the airways to various stimuli, such as allergens, irritants, and viral infections. In individuals with asthma, the airways may respond to these triggers by constricting, leading to the onset or worsening of symptoms. The underlying mechanisms of AHR are not fully understood but are thought to involve a combination of factors, including inflammation, structural changes in the airway walls, and abnormalities in the function of airway smooth muscle cells.
2.2. Airway Remodeling
In addition to inflammation and AHR, airway remodeling is another key feature of asthma. Airway remodeling refers to structural changes that occur in the airways as a result of chronic inflammation. These changes may include thickening of the airway walls, increased smooth muscle mass, deposition of extracellular matrix proteins, and increased mucus production. Airway remodeling can contribute to the persistence and severity of asthma symptoms, as well as the development of airflow obstruction and reduced lung function.
The exact mechanisms driving airway remodeling in asthma are not entirely understood, but various growth factors and cytokines released by inflammatory cells are thought to play a role. These factors can stimulate the proliferation and differentiation of airway structural cells, such as fibroblasts, smooth muscle cells, and epithelial cells, leading to the observed changes in airway structure.
2.3. Immune System Involvement
The immune system plays a central role in the pathogenesis of asthma, particularly in the development of airway inflammation. Asthma is often associated with a dysregulated immune response, characterized by an imbalance between the two main types of T helper (Th) cells, Th1 and Th2. In individuals with asthma, the immune system tends to mount a Th2-dominant response, leading to the production of cytokines, such as interleukin (IL)-4, IL-5, and IL-13, which promote inflammation, mucus production, and AHR.
Allergens, such as pollen, dust mites, and animal dander, are common triggers of asthma symptoms. In susceptible individuals, exposure to these allergens can lead to the activation of the immune system and the production of allergen-specific immunoglobulin E (IgE) antibodies. These antibodies bind to mast cells and basophils, sensitizing them to the allergen. Upon subsequent exposure, the allergen binds to the IgE molecules on the surface of these cells, leading to their activation and the release of inflammatory mediators, such as histamine, which contribute to the development of asthma symptoms.

3. Risk Factors and Causes
3.1. Genetic Factors
Asthma has a complex genetic basis, with multiple genes contributing to an individual’s susceptibility to the disease. Studies have identified various genetic loci and polymorphisms associated with asthma risk, often involving genes related to immune system function, airway inflammation, and structural components of the airways. The heritability of asthma is estimated to be between 35% and 95%, and having a family history of asthma or other atopic diseases, such as allergic rhinitis or eczema, increases an individual’s risk of developing the condition.
3.2. Environmental Factors
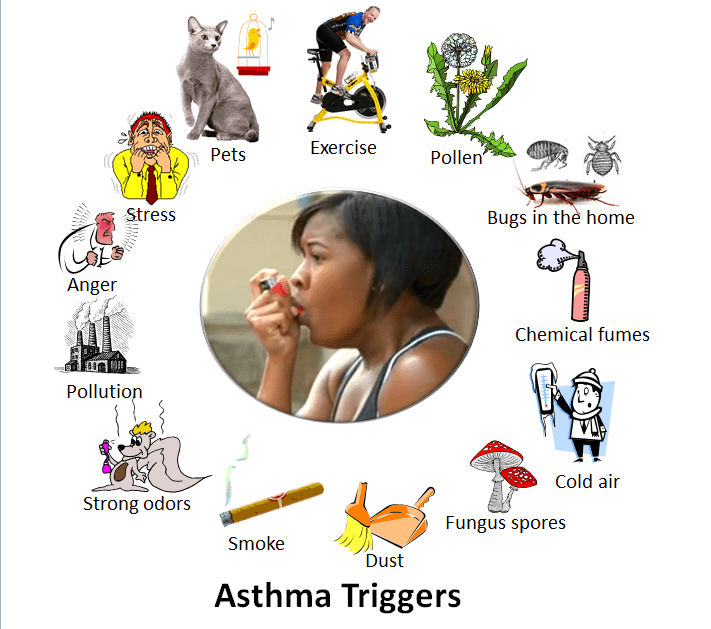
Environmental factors play a significant role in the development and exacerbation of asthma symptoms. Exposure to various indoor and outdoor pollutants, such as tobacco smoke, particulate matter, and ozone, has been associated with an increased risk of asthma and worsening of symptoms in those with the disease. Additionally, exposure to occupational irritants, such as chemicals, dust, and fumes, can lead to the development of occupational asthma, a subtype of the condition.
3.3. Allergens
Allergens are substances that can trigger an allergic reaction in susceptible individuals, leading to the onset or worsening of asthma symptoms. Common allergens associated with asthma include pollen, dust mites, mold spores, and animal dander. Exposure to these allergens can cause the immune system to mount a Th2-dominant response, resulting in the production of allergen-specific IgE antibodies and the release of inflammatory mediators that contribute to airway inflammation and bronchoconstriction.
3.4. Infections
Respiratory infections, particularly those caused by viruses, can trigger asthma symptoms and exacerbations. Infections with viruses such as rhinoviruses, respiratory syncytial virus (RSV), and influenza can cause airway inflammation and increase airway responsiveness, leading to worsening asthma symptoms. Additionally, early-life respiratory infections have been implicated in the development of asthma in children, with some evidence suggesting that viral infections during infancy may predispose individuals to the development of the disease later in life.
3.5. Lifestyle Factors
Various lifestyle factors can influence the risk of developing asthma and the severity of symptoms. Obesity has been associated with an increased risk of asthma, as well as poorer asthma control and reduced response to certain asthma medications. Physical inactivity, poor diet, and stress can also contribute to the development and worsening of asthma symptoms. Furthermore, certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and beta-blockers, can trigger asthma symptoms in susceptible individuals.
4. Diagnosis of Asthma
4.1. Medical History and Physical Examination
The diagnosis of asthma begins with a thorough medical history and physical examination. The healthcare provider will ask about the patient’s symptoms, their frequency and severity, possible triggers, and any personal or family history of asthma or other atopic diseases. The physical examination may include an assessment of the patient’s breathing, use of accessory muscles, and presence of wheezing or other abnormal lung sounds. However, the absence of these findings does not rule out asthma, as symptoms can vary over time and may be absent during the examination.
4.2. Pulmonary Function Tests
Pulmonary function tests (PFTs) are essential tools for diagnosing asthma and assessing lung function. The most common PFT is spirometry, which measures the volume of air inhaled and exhaled, as well as the speed of exhalation. In individuals with asthma, spirometry may reveal airflow obstruction, which is typically reversible with the use of a bronchodilator, such as albuterol. The bronchodilator reversibility test is performed by repeating spirometry after administering a bronchodilator and comparing the results. An improvement in lung function after bronchodilator administration supports the diagnosis of asthma.
4.3. Allergy Testing
Since allergies can be a significant trigger for asthma symptoms, allergy testing may be performed to identify specific allergens that may be contributing to a patient’s asthma. Skin prick testing and blood tests for allergen-specific IgE antibodies are common methods for allergy testing. Identifying and managing exposure to allergens can be an essential component of an individual’s asthma management plan.
4.4. Imaging Techniques
Imaging techniques, such as chest X-ray or computed tomography (CT) scan, are not routinely used for the diagnosis of asthma but may be performed to rule out other conditions that can cause similar symptoms, such as pneumonia, bronchiectasis, or lung tumors. In some cases, imaging may reveal findings suggestive of asthma, such as hyperinflated lungs or bronchial thickening, but these are not specific to the disease and should be interpreted in the context of the patient’s clinical presentation and other diagnostic findings.
4.5. Differential Diagnosis
Several other conditions can cause symptoms similar to those of asthma, and it is essential to consider these when making a diagnosis. Some of the differential diagnoses for asthma include chronic obstructive pulmonary disease (COPD), bronchiectasis, vocal cord dysfunction, gastroesophageal reflux disease (GERD), heart failure, and pulmonary embolism. The healthcare provider will consider the patient’s age, medical history, physical examination findings, and results of diagnostic tests to differentiate between asthma and other conditions. In some cases, additional testing or consultation with a specialist may be required to confirm the diagnosis.

5. Treatment of Asthma
5.1. Pharmacological Treatment
Pharmacological treatment options for asthma aim to reduce inflammation, relieve bronchoconstriction, and manage symptoms. These medications can be classified into two main categories: controllers, which are used for long-term control of asthma, and relievers, which provide quick relief of symptoms during an asthma attack.
5.1.1. Short-Acting Bronchodilators
Short-acting bronchodilators, such as albuterol, are used as reliever medications to quickly reverse bronchoconstriction and alleviate asthma symptoms during an attack. These medications are typically administered via inhalation using a metered-dose inhaler (MDI) or nebulizer and provide rapid relief of symptoms within minutes. Short-acting bronchodilators should be used as needed for symptom relief but not as a substitute for long-term controller medications.
5.1.2. Long-Acting Bronchodilators
Long-acting bronchodilators, such as long-acting beta-agonists (LABAs) and long-acting muscarinic antagonists (LAMAs), are used as controller medications to provide sustained bronchodilation and symptom control. LABAs, such as salmeterol and formoterol, are often used in combination with inhaled corticosteroids (ICS) for moderate to severe asthma, as they can enhance the anti-inflammatory effects of ICS. LAMAs, such as tiotropium, are less commonly used in asthma but may be added as an additional controller medication in cases of severe or uncontrolled asthma.
5.1.3. Inhaled Corticosteroids
Inhaled corticosteroids (ICS), such as fluticasone, budesonide, and beclomethasone, are the cornerstone of long-term controller therapy for asthma. These medications reduce airway inflammation and hyperresponsiveness, leading to improved symptom control and reduced risk of exacerbations. ICS are typically administered via inhalation using an MDI or dry powder inhaler (DPI) and are available in various strengths to accommodate different severity levels of asthma. The dose of ICS should be adjusted according to the patient’s level of asthma control and the lowest effective dose should be used to minimize potential side effects.
5.1.4. Leukotriene Modifiers
Leukotriene modifiers, such as montelukast and zafirlukast, are oral medications that block the action of leukotrienes, inflammatory mediators involved in bronchoconstriction and mucus production. These medications can be used as an alternative or add-on controller therapy for patients with mild to moderate asthma, particularly those with exercise-induced asthma or aspirin-sensitive asthma. Leukotriene modifiers can also be helpful in managing allergic rhinitis, which often coexists with asthma.
5.1.5. Biologics
Biologic therapies are a relatively new class of medications for severe, uncontrolled asthma. These medications target specific immune system pathways involved in the pathogenesis of asthma, such as IgE production or eosinophilic inflammation. Examples of biologics used in asthma treatment include omalizumab (anti-IgE), mepolizumab and reslizumab (anti-IL-5), benralizumab (anti-IL-5 receptor), and dupilumab (anti-IL-4 receptor). Biologics are typically administered as injections and may be considered for patients with severe asthma who do not respond adequately to conventional controller therapies.
5.2. Non-Pharmacological Treatment
5.2.1. Environmental Control and Trigger Avoidance
Identifying and avoiding triggers is an essential component of asthma management. This may include minimizing exposure to allergens, such as dust mites, pet dander, and pollen, as well as avoiding irritants like tobacco smoke and air pollution. Patients should be educated about their specific triggers and strategies for reducing exposure, such as using allergen-proof mattress and pillow covers, maintaining good indoor air quality, and avoiding outdoor activities during peak pollen times or high pollution days.
5.2.2. Asthma Action Plan
An individualized asthma action plan is a written document that outlines the patient’s daily management and how to respond in case of an asthma exacerbation. The action plan should include information about the patient’s medications, including dosages and frequencies, instructions for using inhalers and other devices, and steps to take in case of worsening symptoms or an emergency. Patients should be encouraged to review and update their asthma action plan regularly with their healthcare provider to ensure optimal management.
5.2.3. Breathing Techniques and Exercises
Certain breathing techniques and exercises, such as diaphragmatic breathing, pursed-lip breathing, and Buteyko breathing, can help improve lung function and reduce asthma symptoms. These techniques can help patients gain better control over their breathing and reduce the reliance on rescue medications. Additionally, engaging in regular physical activity can improve overall lung function and reduce asthma symptoms, provided that exercise-induced asthma is appropriately managed.
5.2.4. Allergen Immunotherapy
Allergen immunotherapy, also known as allergy shots, is a treatment option for patients with allergic asthma triggered by specific allergens. This treatment involves the administration of gradually increasing doses of allergens to desensitize the immune system and reduce the severity of allergic reactions. Allergen immunotherapy has been shown to improve asthma control and reduce the need for medications in some patients. However, this treatment may not be suitable for everyone and should be discussed with a healthcare provider to determine if it is an appropriate option.
5.2.5. Patient Education and Self-Management
Education and self-management are crucial aspects of asthma care. Patients should be educated about their condition, the importance of adherence to their medications, proper inhaler technique, and strategies for avoiding triggers. Regular follow-up visits with a healthcare provider are essential for monitoring asthma control, adjusting treatment as needed, and addressing any concerns or questions. Additionally, patients should be encouraged to seek support from asthma education programs, support groups, or online resources to help them better understand and manage their condition.

6. Asthma Complications and Prognosis
6.1. Complications
Poorly controlled asthma can lead to several complications, affecting a patient’s quality of life and overall health. Some of these complications include:
6.1.1. Asthma Exacerbations
Severe asthma exacerbations, or “asthma attacks,” can lead to respiratory failure, hospitalization, or even death. Adequate management of asthma, including adherence to controller medications and avoidance of triggers, is critical to prevent these life-threatening events.
6.1.2. Pneumonia
People with asthma are at a higher risk of developing respiratory infections, such as pneumonia, which can further compromise lung function and exacerbate asthma symptoms. Vaccination and prompt treatment of infections are essential to reduce the risk of complications.
6.1.3. Airway Remodeling
Chronic airway inflammation in asthma can lead to structural changes in the airways, known as airway remodeling. This includes thickening of the airway walls, increased mucus production, and alterations in smooth muscle function. Airway remodeling can result in a progressive decline in lung function and may be irreversible in some cases.
6.1.4. Psychological Impact
Asthma can have a significant impact on a patient’s mental health, with increased rates of anxiety, depression, and sleep disturbances. Proper asthma management and psychological support can help improve the overall well-being of individuals with asthma.
6.2. Prognosis
The prognosis for asthma varies depending on the severity of the disease, the patient’s adherence to treatment, and the presence of other medical conditions. With proper management, many individuals with asthma can lead normal, active lives with minimal symptoms. Some patients may experience a decrease in asthma severity over time, while others may have persistent symptoms or even worsening of their disease.
Several factors can influence the prognosis of asthma, including:
6.2.1. Age of Onset
Early-onset asthma, beginning in childhood, is often associated with allergic triggers and a family history of asthma. Late-onset asthma, which develops in adulthood, is more likely to be severe and less responsive to treatment.
6.2.2. Asthma Severity
Individuals with mild, intermittent asthma typically have a better prognosis compared to those with moderate to severe, persistent asthma. Severe asthma is associated with more frequent exacerbations, hospitalizations, and a higher risk of complications.
6.2.3. Treatment Adherence
Adherence to the prescribed asthma treatment plan, including controller medications and trigger avoidance, is essential for maintaining asthma control and preventing complications. Patients who consistently follow their treatment plan have a better prognosis.
6.2.4. Comorbidities
The presence of other medical conditions, such as obesity, gastroesophageal reflux disease (GERD), or allergic rhinitis, can influence asthma control and prognosis. Managing these comorbidities is an essential aspect of asthma care.
Overall, early diagnosis, appropriate treatment, and patient education are crucial factors in determining the prognosis of asthma and preventing complications. Regular follow-up visits with a healthcare provider can help monitor asthma control and adjust treatment as needed to optimize outcomes.









Wow, I never knew that an asthma attack could trigger chest tightness and coughing. My boss noticed that one of our colleagues has been coughing lately while at work. I’ll be sure to brief this to my boss so he’d consider sending him for asthma treatment when it persists.